Placental Abruption
BMJ Best Practice Clinical Guideline Placental abruption. Last reviewed: Jun 2025.
Disclaimer
There is currently no dedicated NICE guideline specifically addressing placental abruption. The RCOG Green-top Guideline No. 63: Antepartum Haemorrhage (published 2011) includes placental abruption, but its coverage is non-specific and has not been updated in over 10 years.
Therefore, this article is based primarily on BMJ Best Practice clinical guidance.
Background Information
Definition
Separation of the placenta from the uterus prior to delivery.
Causes and Risk Factors
Lifestyle Factors
- Smoking
- Cocaine use (and other stimulants)
- Alcohol misuse
- Low BMI
Maternal Conditions
- Hypertension – most common cause
- Pre-eclampsia
- Autoimmune disease (e.g. antiphospholipid syndrome)
- Thrombophilia
Pregnancy Factors
- Maternal age
- < 20 y/o
- >35 y/o
- Previous placental abruption – strongest risk factor
- Multiple pregnancy
- Trauma to the abdomen
- Polyhydramnios
- Assisted reproductive technologies (e.g. IVF)
Clinical Features
Onset: >20 weeks (esp. third trimester)
Sudden onset of:
- Abdominal pain
- ‘Woody‘ tender uterus
- Vaginal bleeding (may be ‘concealed’ / not be present) – major cause of antepartum haemorrhage
Other:
- Foetal heart rate abnormalities (such as nonreassuring fetal status or fetal distress)
- Severe cases → Maternal shock (tachycardia, hypotension etc.) / DIC
20% cases of placental abruption are concealed where the bleeding is trapped behind the placenta, such that there would be no or minimal vaginal bleeding.
Concealed abruptions can be particularly dangerous, as the severity can be underestimated (visible blood loss can be little, but internal bleeding is significant).
Gudielines
Investigation and Diagnosis
Placental abruption is mainly a clinical diagnosis
Blood Tests
- FBC (including haemoglobin and haematocrit)
- Clotting studies
Imaging
1st line: ultrasound
- May show retroplacental haematoma
- Detection rate is low; ~12-25%
- Negative ultrasound does not exclude abruption
- Useful for excluding placenta praevia (DDx antepartum haemorrhage)
Fetal Monitoring
Perform continuous cardiotography
- Fetal well-being is important in guiding management
Management
Stabilise the mother and resuscitate as needed.
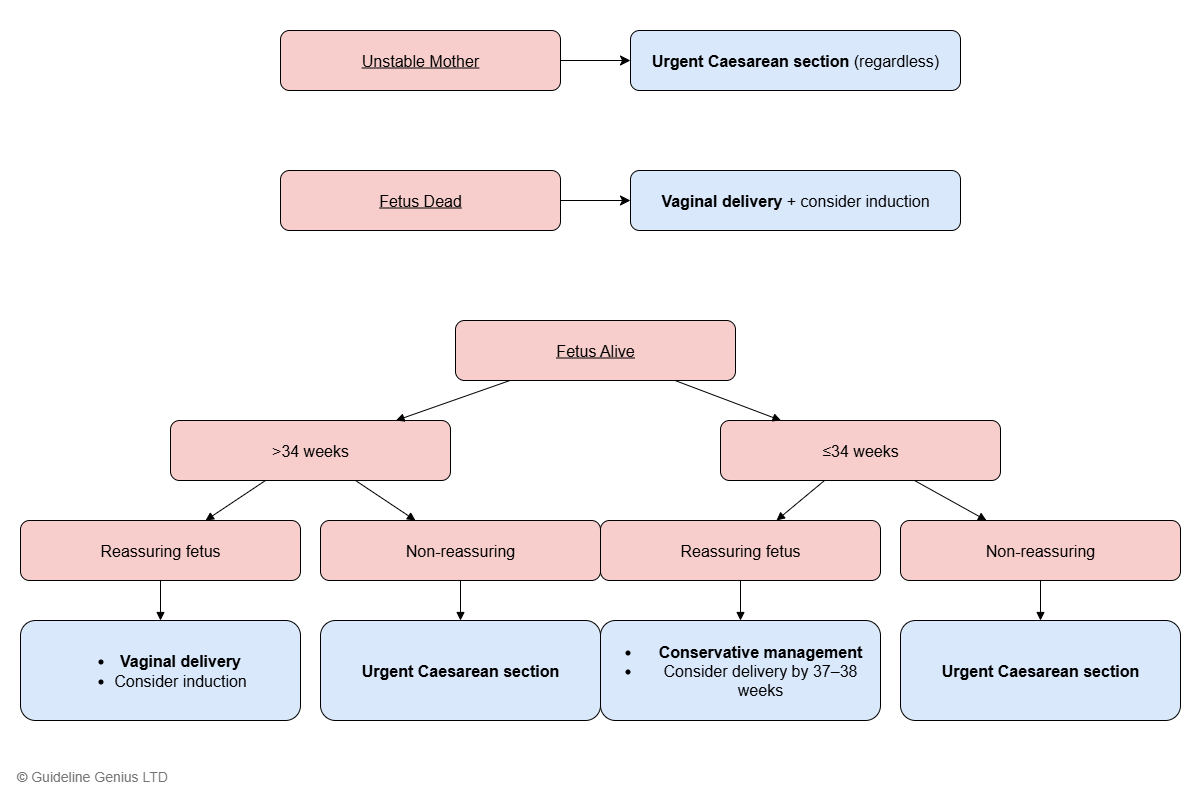
Definitive management depends on 1) fetal status and 2) weeks of gestation, with exceptions:
- Unstable maternal status → urgent Caesarean section (regardless of fetal status and weeks of gestation)
- Intrauterine fetal demise (dead fetus)→ vaginal delivery (usually with induction)
Non-reassuring fetal status is evidenced by several suspicious / abnormal CTG features (further detail on NICE ‘fetal monitoring in labour’): [Ref]
- Fetal bradycardia (baseline heart rate <110 bpm)
- Prolonged decelerations (>3 minutes)
- Late decelerations
- Loss of baseline variability
- Persistent tachycardia
The most critical findings are acute sustained bradycardia or prolonged deceleration, which reflect acute fetal hypoxia and warrant urgent obstetric review for expedited delivery