Ischaemic Stroke
National Clinical Guideline for Stroke 2023 Edition.
NICE Guideline [NG128] Stroke and transient ischaemic attack in over 16s: diagnosis and initial management. Last updated: Apr 2022
This article has been updated to include a simplified emergency department / hospital stroke pathway to provide a clearer context for assessment and initial management.
Minor restructuring has also been done to improve clarity, flow, and readability.
Changes made: 05/11/25
Approach
Refer all suspected cases of stroke to hyperacute stroke service
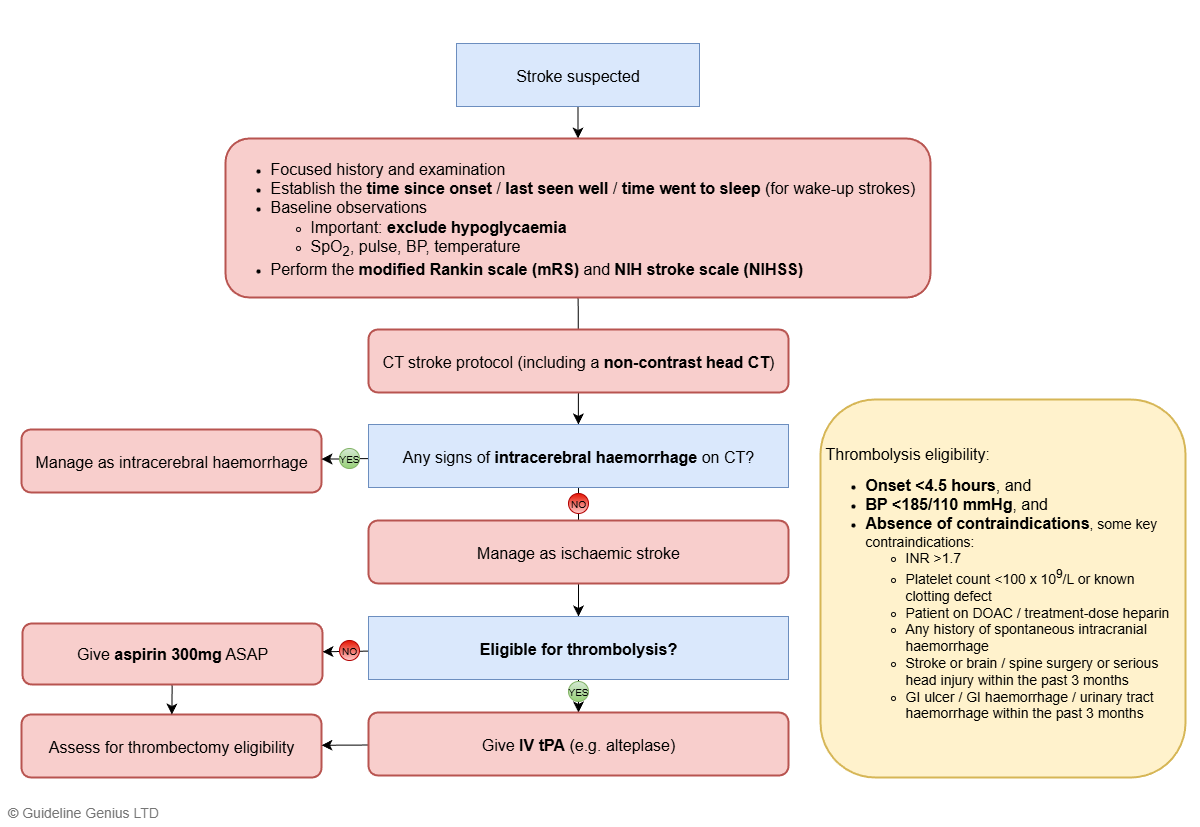
The pathway below illustrates a simplified approach to acute stroke assessment and initial management in the emergency department / hospital setting.
Note that thrombolysis and thrombectomy are 2 independent interventions, with separate indications and contraindications:
- If eligible for both thrombolysis and thrombectomy → thrombolysis should be given without delay and activate the thrombectomy protocol at the same time
Diagnosis
Choice of Imaging
1st line and most important: non-contrast head CT within 1 hour to exclude intracerebral haemorrhage
Further imaging:
- Diagnostic uncertainty → MRI brain with stroke-specific sequences
- Potentially eligible for thrombolysis and/or thrombectomy
- CT / MR perfusion (alternative: MRI measuring DWI-FLAIR mismatch)
- CT angiogram from the aortic arch to skull vertex
If the patient is likely eligible for thrombectomy (e.g. high NIHSS and low modified Rankin score), a CT stroke protocol is usually ordered instead of just a non-contrast head CT
CT stroke protocol includes a sequence of scans: non-contrast CT → CT perfusion → CT angiography, which excludes intracerebral haemorrhage and gives the relevant information needed to assess eligibility for thrombectomy.
Imaging Findings in Stroke
Imaging findings of ischaemic stroke:
| CT head (non-contrast) |
|
| MRI |
MRI can detect very early ischaemic changes (within minutes) |
On CT/MRI, the location of the infarct (hypodensity on CT / hyperintensity on MRI) reflects the arterial territory affected:
- Lateral cortex (away from midline) → MCA infarct
- Medial cortex (near the midline) → ACA infarct
- Occipital lobe → PCA infarct
- Basal ganglia / internal capsule → lenticulostriate vessel infarct (Lacunar stroke)
- Brainstem / cerebellum → vertebrobasilar artery infarct
The initial non-contrast CT head in suspected stroke is NOT performed to confirm ischaemia, but to exclude intracerebral haemorrhage.
If the clinical presentation is consistent with an ischaemic stroke and the CT does not show haemorrhage, then the patient is treated as having an ischaemic stroke.
Note that a CT is often normal in the first few hours after an ischaemic stroke; visible hypodensity may not appear until 12–24 hours after onset. An MRI can detect ischaemic changes within minutes of ischaemia, but should not delay urgent management.
It is important to be aware of the findings of intracerebral haemorrhage on non-contrast CT head
- A hyperdense (bright-white) mass (of the acute blood)
- Surrounded by a hypodense rim (of the surrounding oedema)
Acute Management
Supportive Measures
| Oxygen therapy | Do not give routinely; only if SpO2 <94% |
| Blood glucose | Target: 4-11 mmol/L |
| Swallowing assessment | Screen swallowing before any oral intake (food, fluid, medications)
|
| Blood pressure control | Blood pressure should NOT be routinely lowered in acute ischaemic stroke unless there are specific indications, as this can further compromise cerebral perfusion & neurological outcomes
|
Aspirin
Aspirin 300mg should be offered ASAP once
- Intracerebral haemorrhage has been excluded, and
- Patient is NOT undergoing thrombolysis
If the patient is dysphagic → administer via an enteral / rectal tube
If the decision is made to treat the patient with thrombolysis, aspirin 300mg should only be given 24 hours after thrombolysis (and once repeat imaging excludes haemorrhage).
Do NOT give aspirin before or with thrombolysis.
Thrombolysis
Eligibility
Standard eligibility: < 4.5 hours since symptom onset / last known well
The latest guideline also advised on extended-window eligibility:
- Thrombolysis can be started between 4.5-9 hours of known onset OR within 9 hours of the midpoint of sleep (for wake-up stroke), AND
- Neuroimaging (CT / MR perfusion, or MRI DWI-FLAIR mismatch) shows potential to salvage brain tissue
For UKMLA purposes, it is sufficient to know the standard thrombolysis eligibility of <4.5 hours from symptom onset.
The extended-window thrombolysis criteria (4.5–9 hours / wake-up stroke with advanced imaging) are specialist-led decisions and are unlikely to be tested in the UKMLA.
Contraindications
Key contraindications (not an exhaustive list):
- BP >185/110 mmHg (this is a reversible contraindication → if hypertension is the only contraindication, lower the BP then give thrombolysis)
- Intracranial haemorrhage (should be excluded with non-contrast CT head)
- Haematological bleeding risks
- INR >1.7
- Platelet count <100 x 109/L / known clotting defect
- Patient on DOAC or treatment-dose heparin
- Structural bleeding risks
- Any history of spontaneous intracranial haemorrhage
- Stroke / brain or spine surgery / serious head injury within the past 3 months
- GI ulcer / bleeding within the past 3 months
Thrombolytic Therapy
In order to give thrombolytic therapy, ALL 3 of the following must be met:
- Eligibility criteria met
- No contraindications
- BP <185/110 mmHg
Agent of choice: IV alteplase / tenecteplase
- Drug class: tissue plasminogen activator (tPA)
Thrombectomy (Intra-Arterial Clot Extraction)
Decisions regarding thrombectomy are complicated and are made by a specialist. The general indications for thrombectomy can be categorised into 3 main domains:
- Timing
- Generally speaking, thrombectomy can be done up ot 24 hours from symptom onset / last known well
- Clinical factors
- High NIHSS (i.e. presence of disabling / severe neurological deficits)
- Low mRS (i.e. good pre-stroke functional status)
- Imaging factors
- Proximal vessel occlusion (i.e. large vessel occlusion) (indicated by angiography)
- If there is potential to salvage brain tissue (indicated by CT / MR perfusion)
Eligibility criteria for thrombectomy:
| Offer thrombectomy in proximal anterior circulation occlusion (confirmed on CTA / MRA) if |
|
| Consider thrombectomy in proximal posterior circulation occlusion (confirmed on CTA / MRA) if |
|
NICE recommends that thrombectomy is favoured in:
- Pre-stroke modified Rankin scale <3 (i.e. good pre-stroke functional status)
- NIHSS >5 (i.e. stroke causing disabling / severe neurological deficits)
Decompressive Hemicraniectomy
NICE recommends considering decompressive hemicraniectomy within 48 hours if ALL of the following:
- Clinical features that suggest MCA infarct + NIHSS score >15
- ↓ Level of consciousness + ≥1 on NIHSS item 1a
- MCA territory infarct >50% on CT
Rationale: in malignant MCA infarction, extensive cerebral oedema can develop rapidly. Decompressive hemicraniectomy prophylactically prevents cerebral oedema from raising ICP.
Long-Term Management
All patients should receive the following for secondary prevention:
- High-intensity statin (e.g. atorvastatin 80mg)
- Antithrombotic treatment (antiplatelet or anticoagulation)
- Choice of antiplatelet vs anticoagulation as long-term antithrombotic treatment depends on whether the stroke is associated with atrial fibrillation or not
Patients Without Atrial Fibrillation
- Aspirin 300mg OD continued for 2 weeks after stroke onset
- After 2 weeks → clopidogrel 75mg OD lifelong
- Alternative: aspirin 75mg OD
If the patient is treated with thrombolysis, antiplatelet therapy should be delayed until 24 hours after AND once repeat imaging excludes haemorrhage.
Patients with Atrial Fibrillation
- Offer aspirin 300mg OD initially, until anticoagulation is started
- Start anticoagulation 5-14 days after stroke onset (if the stroke is mild, it’s possible to start anticoagulation less than 5 days after stroke onset)
- 1st line for most patients: DOAC (e.g. apixaban)
- 1st line in valvular AF: warfarin
Note the timing to start anticoagulation in TIA is different from that in ischaemic stroke:
- In ischaemic stroke with AF, anticoagulation is only started after 5-14 days, with aspirin 300mg being given during those 5-14 days
- In TIA with AF, anticoagulation can be started immediately, once intracerebral haemorrhage has been excluded
This difference in timing reflects the balance of benefits and bleeding risk in the presence of established infarction (stroke) vs TIA. Anticoagulants carry a much higher risk of intracerebral haemorrhage than antiplatelets.
In ischemic stroke with AF, there is a significant risk of hemorrhagic transformation in the infarcted brain tissue if anticoagulation is started immediately. Therefore, anticoagulation is typically delayed for about 5-14 days, while aspirin 300 mg is given in this period to prevent early recurrent ischemia.
In TIA with AF, there is no established infarcted tissue and thus essentially no risk of hemorrhagic transformation. Once intracerebral haemorrhage is excluded by imaging, anticoagulation can be started immediately to provide early secondary stroke prevention.
But ultimately, for both ischaemic stroke and TIA patients with AF, long-term anticoagulation (not antiplatelet) is required for effective stroke prevention.
DVLA Guidelines
Driving and Stroke
After a stroke / TIA → always stop driving immediately. Further action depends on the license type:
- Class I vehicle (car / motorcycle)
- Stop driving for at least 1 month
- No need to inform the DVLA routinely (unless there is residual neurological / cognitive deficit after 1 month or there was any seizure or brain surgery was performed)
- Class II vehicle (bus / coach / lorry)
- Must inform the DVLA
- Stop driving for at least 1 year (12 months)
References