Induction of Labour
NICE guideline [NG207] Inducing labour. Published: Nov 2021.
Guidelines
Indications for Inducing Labour
- >41 weeks gestation (due to ↑ risk of stillbirth and Caesarean birth)
- P-PROM at 34-37 weeks – see this article for more details
- If 34-37 weeks → offer induction of labour now OR expectant management until 37 weeks
- If <34 weeks → do not offer induction unless there are additional indications
- Prelabour rupture of membrane at term
- Offer induction of labour now OR induction after 24 hours (if labour not naturally started)
- GBS +ve status if
- P-PROM at 34-37 weeks → induction now OR Caesarean birth
- Prelabour rupture of membrane at term → induction now OR Caesarean birth
- Maternal request
- Intrauterine fetal death
Counsel women with previous Caesarean birth about the risks of induction of labour:
- Risk of uterine rupture
- Increased risk of emergency Caesarean birth
Assessment and Monitoring
Assessment Before Induction
- Assess fetal head position and engagement:
- Abdominal palpation
- If uncertain (e.g. breech suspected) → ultrasound
- Vaginal examination to calculate the Bishop score (see details below)
- Perform cardiotocography to confirm:
- Normal fetal heart rate pattern, and
- Absence of significant uterine contractions (to rule out labour or hyperstimulation)
Monitoring During Induction
Once contraction begins after induction → cardiotocography monitoring
- If normal and low risk → switch to intermittent auscultation
- If abnormal fetal heart rate / uterine hyperstimulation → continuous cardiotocography + stop further induction doses and remove if possible
Methods of Labour Induction
Membrane sweep
Timing: offer the woman an option of membrane sweeping after 39 weeks
Membrane sweep counselling:
- Procedure performed during vaginal examination: a finger is inserted into the cervix to perform a circular sweeping motion, attempting to separate the amniotic sac membrane from the uterine wall
- Underlying mechanism: this stimulates the release of prostaglandins which helps to soften and open the cervix
- Possible side effects: discomfort, light bleeding / cramping, but generally safe
Membrane sweep is NOT a formal induction method but can reduce the need for formal induction (i.e. labour is more likely to start without the need for additional pharmacological or mechanical methods of induction).
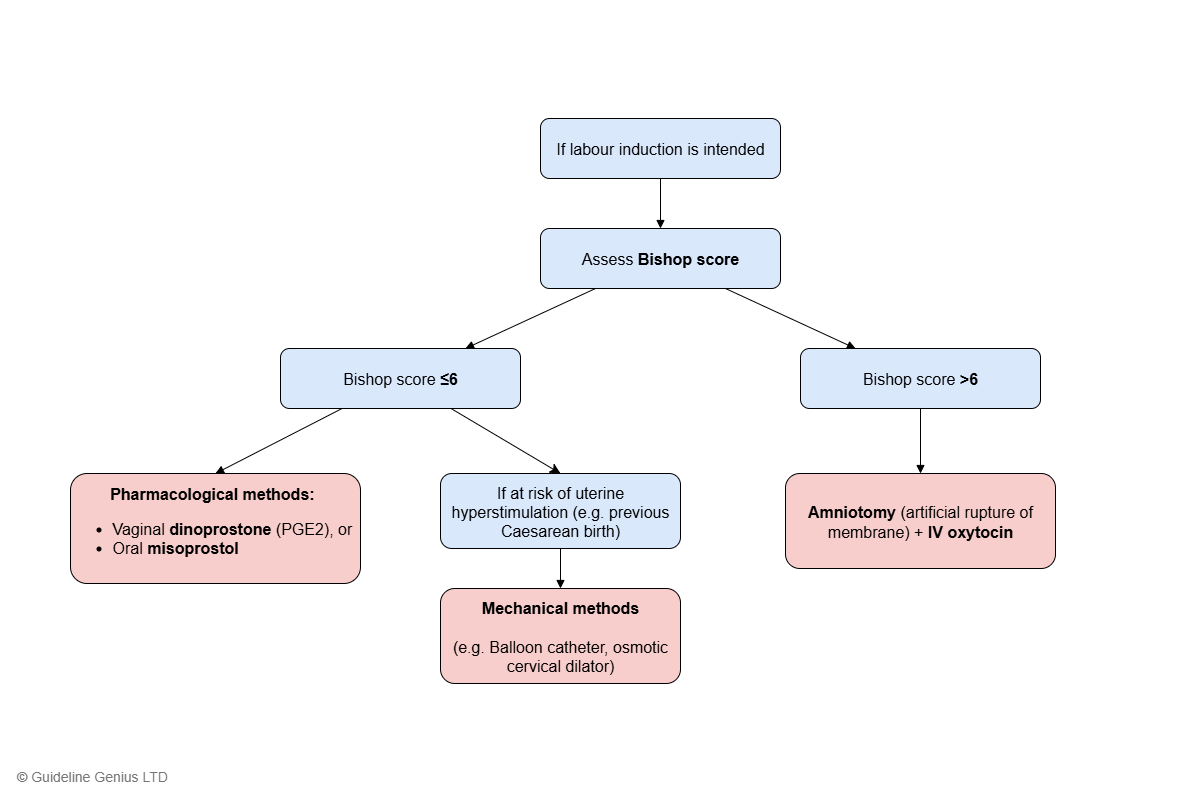
Bishop Score Guided Decision Algorithm
If labour induction is intended, the Bishop score is used to decide which method to use:
| Score | Cervix dilation (cm) | Cervix position | Cervical effacement (%) | Cervical consistency | Fetal station |
|---|---|---|---|---|---|
| 0 | 0 | Posterior | 0-30 | Firm | -3 |
| 1 | 1-2 | Midposition | 40-50 | Moderately firm | -2 |
| 2 | 3-4 | Anterior | 60-70 | Soft | -1,0 |
| 3 | ≥5 | ≥80 | +1,+2 |
Bishop score interpretation:
- ≥8: indicates a favourable / ripe cervix (i.e. cervix is ready to dilate)
- 6: cut-off to determine the choice of induction method
Bishop Score ≤6 → Cervical Ripening Methods
Offer pharmacological induction methods:
- Topical dinoprostone (PGE2) as vaginal tablet / gel / vaginal delivery system, or
- Oral misoprostol (low dose 25 mcg)
Consider mechanical methods (e.g. balloon catheter, osmotic cervical dilator) if any of the following:
- High risk of uterine hyperstimulation and/or uterine rupture
- e.g. previous Caesarean birth, multiple pregnancy, complex uterine scars, history of uterine rupture
- Patient preference
Rationale: Bishop score ≤6 indicates an unfavourable cervix for labour, therefore cervical ripening methods are used to further prepare the cervix before active labour can be safely and effectively induced.
Bishop Score >6 → Labour Stimulating Methods
Offer induction with:
- Amniotomy, and
- IV oxytocin infusion
Rationale: Bishop score >6 indicates that the cervix is ripe and ready for labour, therefore there is no need to further ripen the cervix and labour can be directly stimulated.
Uterine Hyperstimulation
Uterine hyperstimulation is defined by:
- Tachysystole: >5 contractions per 10 min for at least 20 min, and
- Hypersystole / hypertonicity: contraction lasting ≥2 min
Management:
- Stop giving further induction medication
- Remove vaginally administered products if possible
- Perform continuous cardiotography
- Consider tocolysis
Hyperstimulation caused by misoprostol may be more difficult to reverse.
Mechanical methods are less likely to cause hyperstimulation than pharmacological methods.
Outpatient Labour Induction
For those who wish to return home, with no contraindications, consider:
- Vaginal dinoprostone or
- Mechanical methods
Ask the women to contact their maternity team if ANY of the following:
- Contraction begins
- No contractions in an agreed timeframe
- Membrane ruptures
- Bleeding develops
- Any other concerns (e.g. reduced fetal movement, excessive pain or contractions, side effects)