Newborn Life Support (NLS)
Resuscitation Council UK Newborn resuscitation and support of transition of infants at birth Guidelines 2025
Changes made to this article:
- Link to the latest 2025 Resuscitation Guidelines updated
- Minor optimisations made to the flowchart
There were no major changes in the 2025 Resuscitation Council UK guidelines that affect UKMLA-relevant content
Date: 24/11/25
Background Information
APGAR score
APGAR score should be recorded routinely at 1 min and 5 min after birth
| Component | 0 points | 1 points | 2 points |
|---|---|---|---|
| Appearance | Blue / pale completely | Peripheral cyanosis only | Pink |
| Pulse (heart rate) | 0 | <100 | >100 |
| Grimace (reflex irritability) | No response to stimulation | Weak cry when stimulated | Strong cry when stimulated |
| Activity (tone) | Floppy | Some flexion | Active movement |
| Respiration | No breathing | Slow / irregular breathing | Strong cry |
NLS Guidelines
Key Concepts
Inflation vs Ventilation Breaths
| Inflation breaths |
|
| Ventilation breaths |
|
Most causes of resuscitation in newborns are respiratory problems, instead of cardiac problems. More emphasis is put on optimising ‘Breathing’, if not managed well, any subsequent interventions (including CPR) would be ineffective.
CPR in NLS
CPR (chest compression to ventilation ratio of 3:1) should only be started if the heart rate is <60 bpm after 30 seconds of good quality ventilation
Do not mix up the CPR ratios in various age groups:
- Neonates (0-28 days): 3:1
- Children (1 month – puberty): 15:2
- Adults: 30:2
Drugs in NLS
IV adrenaline (1:10,000) 0.2 mL/kg should be given after 30 seconds of effective ventilation and chest compression for 30 sec
Other drugs to consider:
- Glucose – to reduce the likelihood of hypoglycaemia in prolonged resuscitation
- Isotonic crystalloid / O -ve blood – for suspected blood loss or shock unresponsive to other resuscitative measures
- Sodium bicarbonate – for prolonged unresponsive resuscitation with intracardiac acidosis
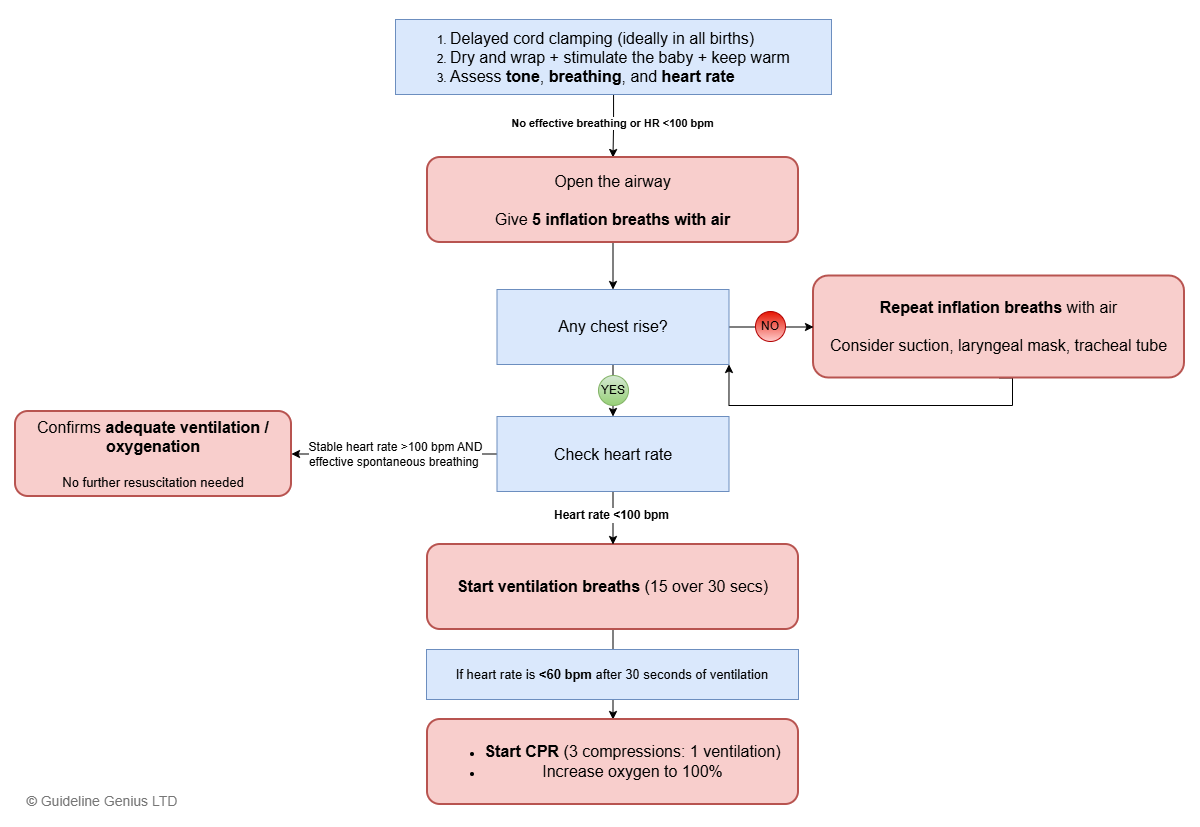
NLS Algorithm
Discontinuing Resuscitation
Discuss stopping resuscitation if there has been no response after 20 minutes and reversible causes have been excluded.