Subarachnoid haemorrhage (SAH)
NICE guideline [NG228] Subarachnoid haemorrhage caused by a ruptured aneurysm: diagnosis and management. Published Nov 2022
NICE states that the guideline only covers the scope of aneurysmal SAH (i.e. SAH secondary to a ruptured aneurysm).
Guidelines
Clinical Assessment
Important red flag symptom for SAH: ‘thunderclap’ headache
Other features of SAH:
- Meningism (triad of neck stiffness + photophobia + headache)
- Limited / painful neck flexion
- Nausea and vomiting
- Altered brain function
Investigation and Diagnosis
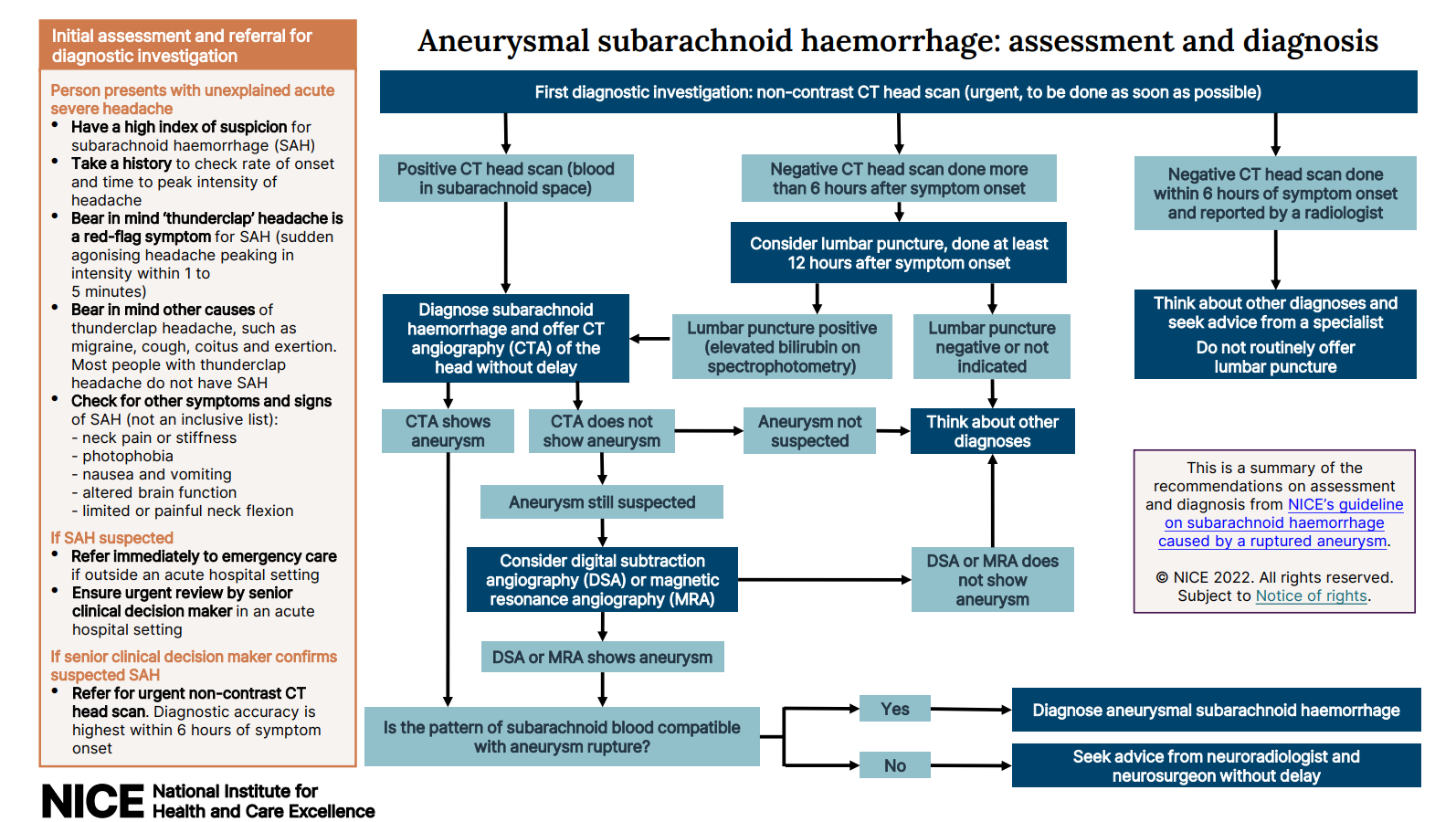
The diagnostic pathway can be split into 2 steps:
- First, confirm SAH
- Then, confirm whether SAH is secondary to an aneurysm or not
1. Diagnosing SAH
1st line investigation: non-contrast CT head ASAP
- Scan +ve → diagnose SAH
- Scan -ve → subsequent actions depend on the timing of the scan is done
6 hours is the cut-off to guide subsequent actions if CT is unable to diagnose SAH:
- Scan done within 6 hours → consider alternative diagnosis (SAH unlikely)
- Scan done after 6 hours → lumbar puncture to be performed at least 12 hours after symptom onset
- If lumbar puncture +ve → diagnose SAH
- If lumbar puncture -ve → consider alternative diagnosis (SAH unlikely)
In short, SAH can be diagnosed in the following scenarios:
- CT head showing blood in the subarachnoid space
- -ve CT head that is performed >6 hours after symptom onset but a +ve lumbar puncture (xanthochromia), that is performed >12 hours after symptom onset.
Non-contrast head CT’s diagnostic accuracy for SAH is highest within 6 hours of symptom onset. After 6 hours, it is less reliable in diagnosing SAH, therefore LP is needed to rule in / rule out SAH.
Why LP should be performed 12 hours after? It takes time for blood to be broken down into bilirubin to give xanthochromia.
Process of lumbar puncture in the context of SAH:
- 3 tubes of CSF is collected to assess for SAH vs traumatic tap
- SAH is diagnosed by the presence of xanthochromia
- Traumatic tap is suggested by declining RBC count across tube 1 to 3
NB that RBC counts CANNOT be used to diagnose SAH, no absolute RBC cut-off reliably diagnose SAH.
2. Diagnosing aneurysmal SAH
The following should be performed without delay once SAH is confirmed:
- 1st line: CT angiography
- 2nd line: MR angiography / digital subtraction angiography
It is important to determine whether SAH is secondary to a ruptured aneurysm or not, as it would affect management.
Management (Aneurysmal SAH)
Pharmacological Management
Nimodipine (oral route preferred over IV)
- Calcium channel blocker
- Prevents vasospasm secondary to SAH
Do not offer pharmacological VTE prophylaxis to people with ruptured cranial vascular malformations (for example, brain aneurysms) or people with intracranial haemorrhage (spontaneous or traumatic) until the lesion has been secured or the condition has stabilised.
Interventional Management – Definitive
Options:
- Endovascular coiling (minimally invasive procedure performed by interventional neuroradiologist) – catheter guided to the aneurysm and coils are placed to promote thrombosis within the aneurysm sac.
- Neurosurgical clipping (open surgery performed by neurosurgeon) – via craniotomy, a clip is placed at the neck of the aneurysm.
- No intervention with monitoring
If interventional treatment is planned, ensure that it is carried out at the earliest opportunity to prevent rebleeding. Be aware that the risk of rebleeding is highest within 24 hours of the onset of symptoms.
Regarding the choice between endovascular coiling and neurosurgical clipping, NICE guideline does not explicitly state a preference, instead it emphasises planning based on 1) aneurysm characteristics, 2) patient factors, 3) availability of expertise. The AHA guideline advocates the same but also provides some extra points:
- Endovascular coiling is often preferred for aneurysms located in the posterior circulation or with narrow necks
- Neurosurgical clipping might be more appropriate for aneurysms with wide neck / complex configurations