Hypertension (Primary)
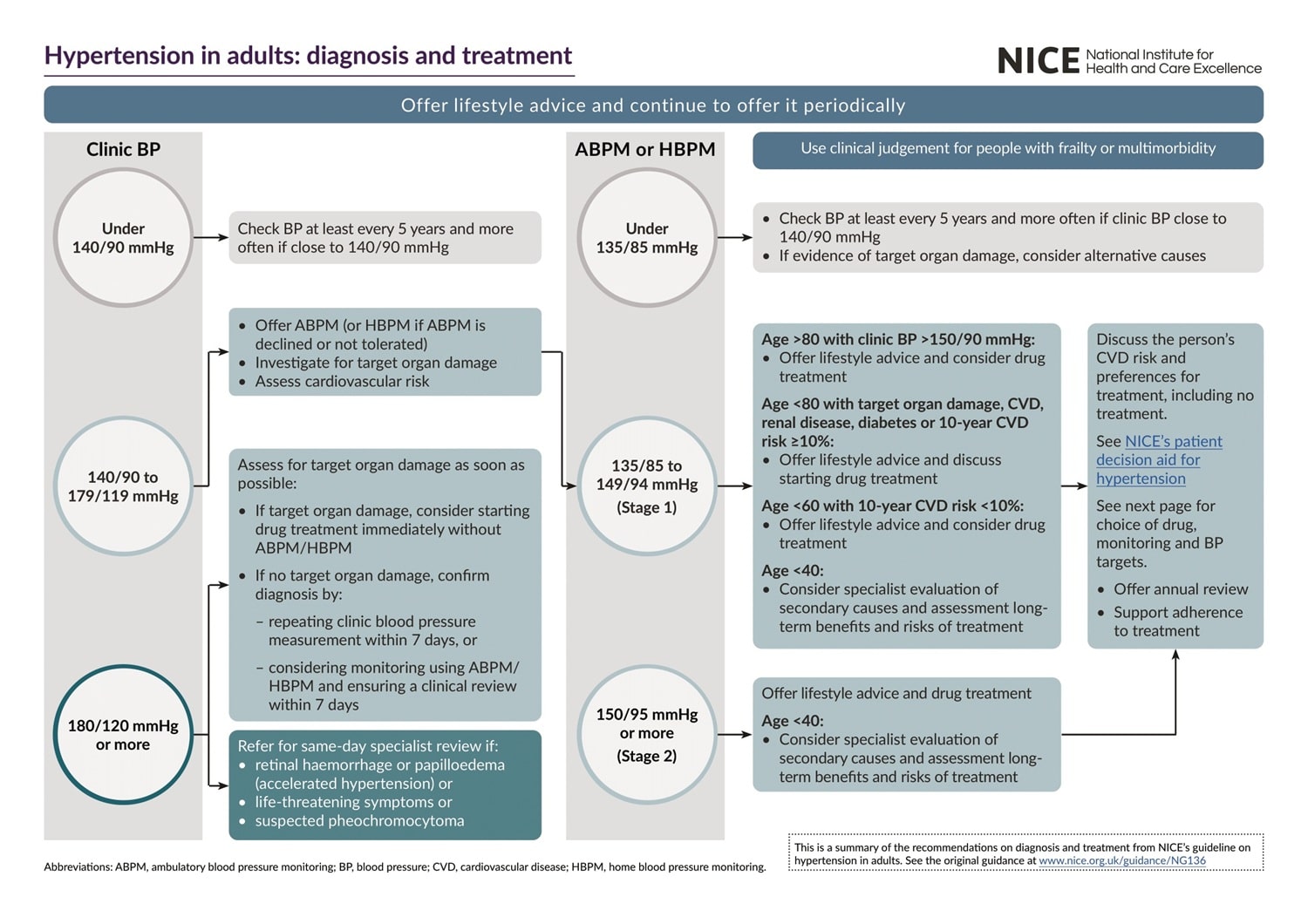
NICE guideline [NG136] Hypertension in adults: diagnosis and management. Last updated: Nov 2023
Background Information
Definition
NICE defines hypertension as:
- ≥140/90 mmHg persistent clinical reading, OR
- ≥135/85 mmHg on 24-hour blood pressure average reading
It is worth noting that the ACC/AHA (US) guidelines differ slightly from NICE (UK) and ESC/ESE/ESO (EU), which recommend a somewhat lower threshold of >130/80 mmHg.
A few important types of hypertension:
- Primary hypertension (essential hypertension): persistently raised BP without an identifiable underlying cause
- Secondary hypertension: persistently raised BP in the presence of an identifiable underlying cause
- Accelerated / malignant hypertension: BP ≥180/120 mmHg + signs of retinal haemorrhage and/or papilloedema
- Resistant hypertension: BP ≥140/90 mmHg, despite triple drug therapy
Staging of Hypertension
The staging of hypertension is important in guiding management and stratifying severity.
| Hypertension stage | Clinical reading cut-off | ABPM / HBPM cut-off |
|---|---|---|
| Stage 1 | ≥140/90 mmHg | ≥135/85 mmHg |
| Stage 2 | ≥160/100 mmHg | ≥150/95 mmHg |
| Stage 3 | ≥180/120 mmHg | N/A |
Clinical Features
Typically asymptomatic and diagnosed on incidental findings.
Possible clinical features in severe hypertension or even malignant hypertension:
| System | Clinical features |
|---|---|
| Head (CNS) |
|
| Eye (hypertensive retinopathy) |
|
| Heart (hypertensive heart disease) |
|
| Kidney (hypertensive nephropathy) |
|
It is important to screen for these features suggestive of severe hypertension and target organ damage. Use a head-eye-heart-kidney approach (from top to bottom) to help remember what to ask.
Diagnosis
Measuring Blood Pressure
Always measure BP in both arms:
- If difference >15 mmHg → repeat measurements
- If difference remains >15 mmHg → measure and record BP in the arm with the higher reading
If clinic BP ≥140/90 mmHg:
- Repeat the measurement → record the lower reading
Investigation and Diagnosis
The approach largely depends on the recorded clinic BP, and importantly referring patients as needed.
Stage 3 Hypertension (BP >180/120 mmHg)
Immediately assess for:
- Retinal haemorrhage or papilloedema (presence of any indicates malignant / accelerated hypertension)
- Life-threatening symptoms
- New-onset confusion
- Chest pain
- Signs of heart failure
- Signs of AKI
Subsequent actions:
- If any of the above is present → refer for same-day specialist assessment
- If referral not indicated → urgent investigation for target organ damage
- Target organ damage present → consider starting drug treatment immediately without confirming diagnosis
- No target organ damage → repeat clinic BP within 7 days OR ABPM / HBPM
Stage 1-2 Hypertension (BP 140-90 – 180/120 mmHg)
Perform the following: (see below for more details)
- Confirm hypertension diagnosis
- Assess for target organ damage
- Assess cardiovascular risk
1. Confirm Hypertension Diagnosis
1st line: ambulatory blood pressure monitoring (ABPM)
- ABPM involves wearing a portable BP cuff under the clothes for 24 hours, while the person carry on normal daily activities and sleep
- The cuff automatically record BP regular intervals – ≥2 measurements/hour during person’s waking hours
- To confirm hypertension: use average of ≥14 measurements taken during person’s waking hours
2nd line: home blood pressure monitoring (HBPM)
- For each recording: take 2 consecutive measurements, ≥1 minute apart with the person seated
- Record BP twice daily (ideally morning and evening)
- Record BP for at least 4 days (ideally 7 days)
- To confirm hypertension: discard recording from day 1 (practice day), use average of all the remaining measurements
Diagnosis of hypertension is confirmed if:
- Clinic BP ≥140/90 mmHg, AND
- ABPM / HBPM average ≥135/85 mmHg
Although NICE recommends ABPM as 1st line to confirm hypertension, quite often HBPM is used as 1st line as ABPM is less practical.
2. Assess for Target Organ damage
Perform all the following:
- Fundoscopy (to check for hypertensive retinopathy)
- 12-lead ECG
- Bloods: HbA1c, U&E, eGFR, total and HDL cholesterol
- Urine: ACR and reagent strip to test for haematuria
3. Assess Cardiovascular Risk
NICE recommends QRISK3 tool to estimate 10-year risk of CVD in 25-84 y/o patients without cardiovascular diseases.
See the Lipid Lowering Therapy and Cardiovascular Risk Reduction article to see how to manage cardiovascular risk and how to manage patients with established cardiovascular diseases.
BP <140/90 mmHg
Check BP at least every 5 years or more often.
Management
Approach
All patients: advise on lifestyle interventions
- A healthy balanced diet, including ↓ dietary sodium intake
- Healthy exercise pattern
- Avoid excessive consumption of caffeine
- Smoking cessation
- ↓ Alcohol consumption
Only start drug therapy in:
- Stage 2 hypertension (regardless of age)
- Stage 1 hypertension + <80 y/o + ANY of the following
- QRISK3 ≥10%
- Target organ damage
- Established CVD
- Diabetes
- Renal disease
Additional recommendations from NICE (less likely to be examined as these are less clean-cut):
- Consider antihypertensive drug treatment in addition to lifestyle advice for <60 y/o with stage 1 hypertension and an estimated QRISK3 <10%
- Consider antihypertensive drug treatment in addition to lifestyle advice for >80 y/o with stage 1 hypertension if clinic BP >150/90 mmHg
- For <40 y/o with hypertension, consider seeking specialist evaluation of secondary causes of hypertension and a more detailed assessment of the long-term balance of treatment benefit and risks. See the Secondary Hypertension article for more information.
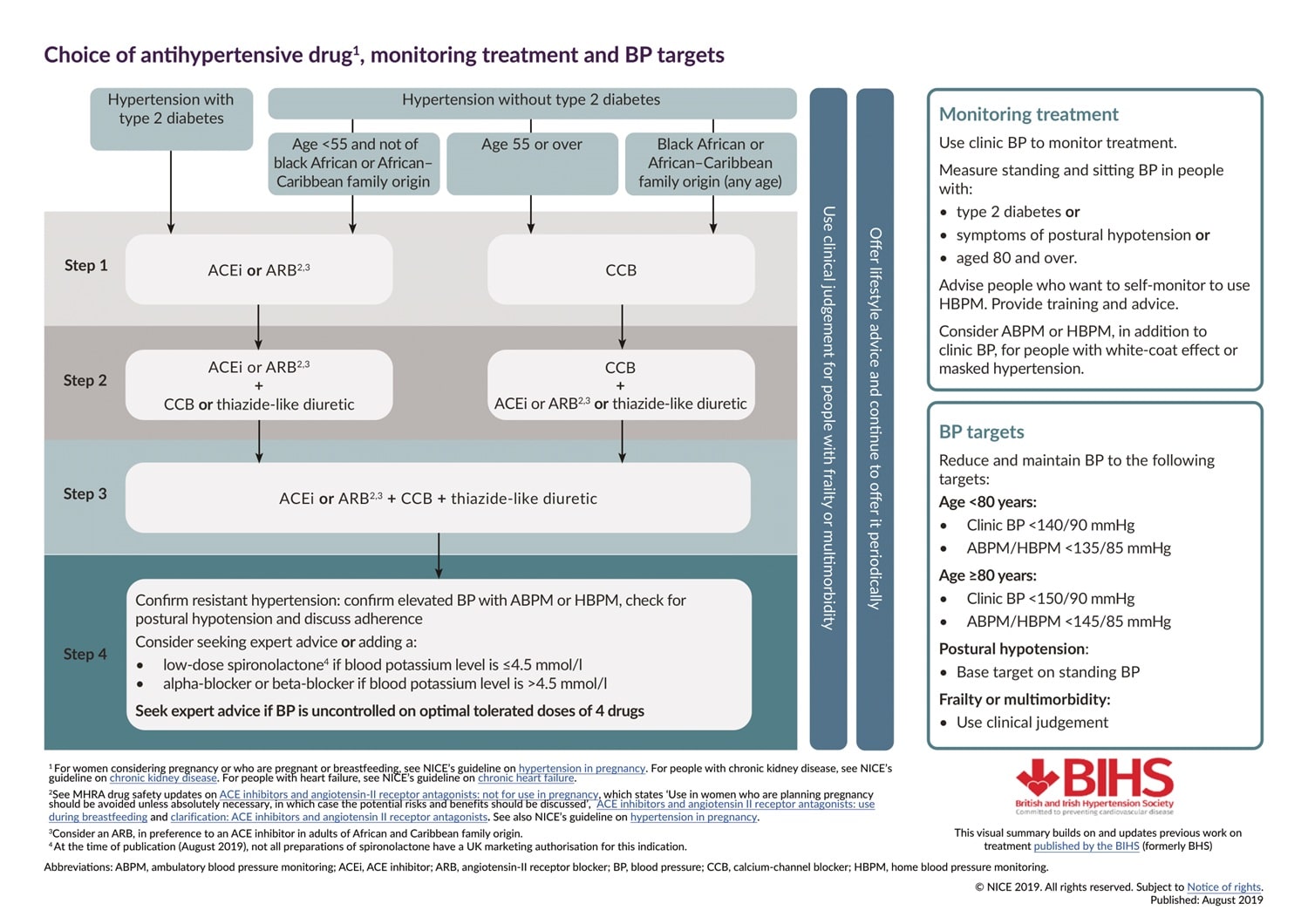
Choice of Anti-Hypertensive Drugs
Examples of commonly used anti-hypertensive drugs:
| Abbreviation | Full form | Drug Examples |
|---|---|---|
| ACE-I | Angiotensin-converting enzyme inhibitor | Ramipril Enalapril Perindopril |
| ARB | Angiotensin receptor (II) blocker | Losartan Valsartan |
| CCB | Calcium channel blocker (dihydropyridine) | Amlodipine Nifedipine |
| Thiazide-like diuretic | N/A | Indapamide
**Thiazide diuretics (e.g. bendroflumethiazide) are fading out are not no longer recommended due to its extensive side effect profile |
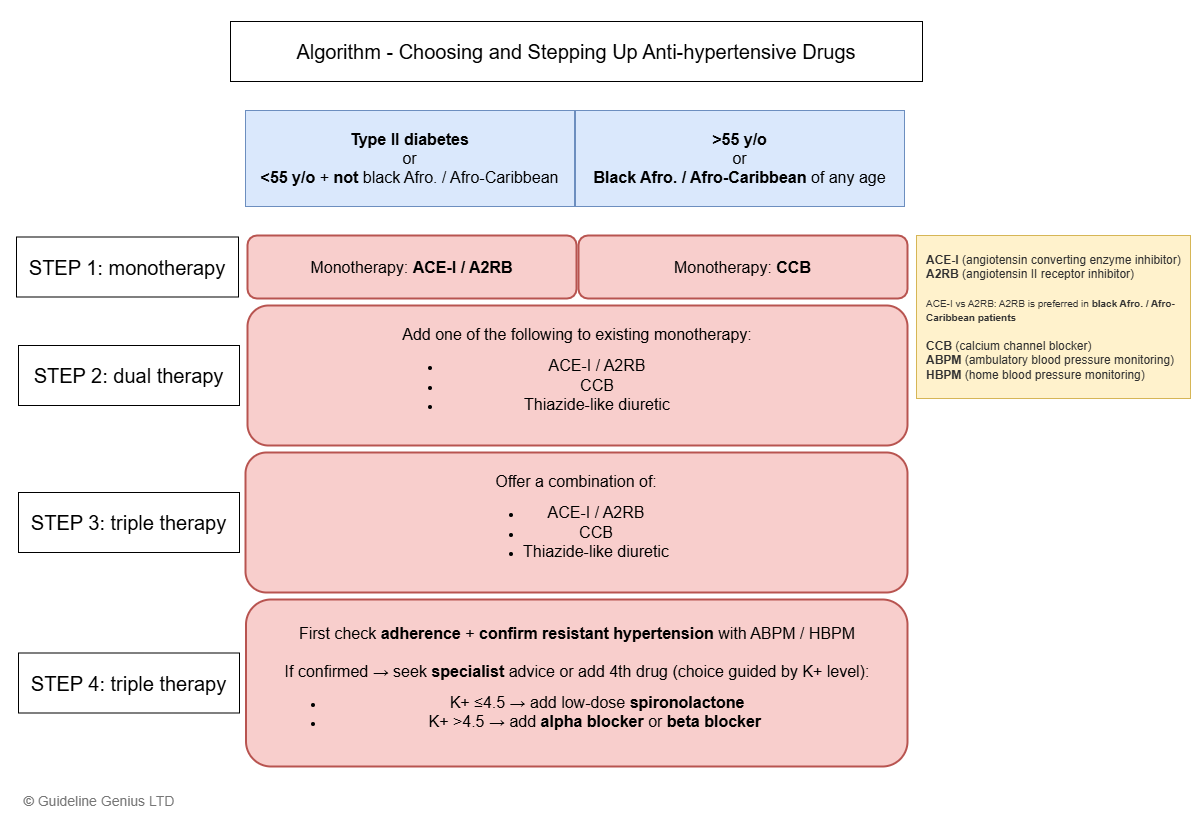
Step 1 – Monotherapy
- If T2DM (regardless of anything) → ACE-I / ARB
- No T2DM
- >55 y/o → CCB
- Afro-Caribbean of any age → CCB
- <55 y/o and NOT Afro-Caribbean → ACE-I / ARB
If there is hypertension + CKD → ACE-I / ARB is preferred for renal protection
Step 2 – Dual Therapy
Add 1 of the following to the current regimen (depending on what the patient is already taking):
- ACE-I / ARB
- CCB
- Thiazide-like diuretic
Step 3 – Triple Therapy
Give a combination of:
- ACE-I / ARB
- CCB
- Thiazide-like diuretic
Step 4 – Quadruple Therapy
First, perform the following:
- Confirm resistant hypertension with ABPM or HBPM
- Discuss adherence to medication
- Check for postural hypotension
For confirmed resistant hypertension → seek specialist advice / add a 4th drug (choice depends on blood potassium level):
- Potassium ≤4.5 mmol/L → spironolactone (low-dose)
- Potassium >4.5 mmol/L → alpha blocker (e.g. doxazosin) / beta blocker (e.g. atenolol, bisoprolol)
Always seek specialist advice if BP is not controlled with 4 drugs.
The rationale of choosing the 4th anti-hypertensive drug depends on the risk of hyperkalaemia:
- Spironolactone is a potassium-sparing diuretic, therefore it is reasonable to only add it if the potassium level is on the low side (reference range 3.5-5.5 mmol/L)
- If the potassium level is on the high side, avoid spironolactone and give something else (i.e. alpha blocker or beta blocker)
Choice of Anti-hypertensive Drugs in Specific Patient Populations
- Black African or African-Caribbean family origin: ARB is preferred over ACE-I
- Patients with hypertension + CKD + ACR >30 mg/mmol → ACE-I / ARB as 1st line
- If ACR ≤30 mg/mmol → follow the above algorithm
- Pregnant patients → see separate article (ACE-I and ARB are teratogenic and should be stopped)
Monitoring and BP Targets
Hypertension patients without T1DM / CKD:
| Age | Clinic BP target (mmHg) | ABPM / HBPM target (mmHg) |
|---|---|---|
| <80 y/o | <140/90 | <135/85 |
| ≥80 y/o | <150/90 | <145/85 |
T1DM / CKD patients:
- <80 y/o
- T1DM / CKD + ACR <70 mg/mmol target: <140/90 mmHg
- T1DM / CKD + ACR ≥70 mg/mmol target: <130/80 mmHg
- ≥80 y/o
- All T1DM (regardless of ACR): <150/90 mmHg
- CKD + ACR <70 mg/mmol target: <140/90 mmHg
- CKD + ACR ≥70 mg/mmol target: <130/80 mmHg
In <80 y/o patients with hypertension, the BP target is the same, irrespective of T1DM and CKD status.
However, when there is T1DM / CKD + ACR ≥70 mg/mmol (indicative of renal impairment), then the BP target is lower (<130/80 mmHg) to prevent deterioration of renal function
The reason why BP targets are higher (or more relaxed) in older individuals is primarily due to the risk of postural hypotension and the risk of falls. The risk of falls outweighs the benefit of optimal BP control in older patients. Importantly, take individual patient factors into account and use clinical judgment.