Asthma (Chronic)
NICE guideline [NG245] Asthma: diagnosis, monitoring and chronic asthma management (BTS, NICE, SIGN). Published: 27 Nov 2024
Key 2024 guideline change:
- Major changes to diagnostic pathway (step 1 now FeNO or blood eosinophil test) (see the full article for more details)
- Major changes to >12 y/o management algorithm (step 1 now anti-inflammatory reliever therapy) (old: SABA monotherapy)
Users are strongly recommended to go over the entire article bit by bit, and major changes were made compared to the old guideline.
Background Information
Definition
Asthma: Asthma is a chronic respiratory condition characterised by chronic airway inflammation and airway hyper-responsiveness to variable triggers, presenting with recurrent symptoms such as wheeze, breathlessness, chest tightness, and cough. It is defined by variable expiratory airflow limitation that is typically reversible, either spontaneously or with treatment. [Ref]
Atopy: Genetic predisposition to produce immunoglobulin E (IgE) antibodies in response to common environmental allergens, leading to an increased risk of developing immediate-type hypersensitivity reactions and clinical syndromes such as atopic dermatitis, allergic rhinitis, and asthma (collectively known as the atopic triad). [Ref]
Epidemiology
Prevalence: ~ 6.5% of the UK population >6 yrs
Age of onset: typically in childhood / young adults
Sex:
- ♂ > ♀ in <18 yrs
- ♀ > ♂ in >18 yrs
Associated comorbidities: [Ref]
- Atopic disorders: allergic rhinitis, atopic dermatitis, chronic rhinosinusitis
- GORD
- Obesity / OSA
- Allergic bronchopulmonary aspergillosis (ABPA)
Aetiology
Multifactorial → Combination of genetic factors, Immune dysregulation (esp. type 2 inflammation), environmental exposures → Chronic airway inflammation & hyperresponsiveness → Asthma symptoms [Ref]
Risk Factors
Risk factors for developing asthma / persistent symptoms:
- Genetic / Host-related
- Personal / family history of atopy
- Perinatal factors: preterm birth, low birth weight
- Overweight / Obesity
- Environmental / Lifestyle Exposure
- Smoking: Active/passive (including e-cigarettes)
- Allergens (if sensitised): House dust mites, pets, pollens, moulds, foods
- Other exposures: Air pollution, noxious chemicals, fungal spores
Triggers
Known Triggers of asthma symptoms / exacerbations
- Viral URTIs
- Exercise
- Exposure to cold air
- Anxiety or strong emotions (i.e, laughter/crying)
- Weather changes
- Drugs
- Beta-blockers
- Aspirin
- NSAIDs
- Occupational triggers → occupational asthma
- Most commonly: airborne allergic sensitisation to flour dust or isocyanates
Complications and Prognosis
Complications
- Acute exacerbations (asthma attacks)
- Leading cause of asthma-related morbidity & mortality. [Ref]
- Respiratory complications
- Acute: pneumomediastinum, pneumothorax, pneumonia, hypercapnic respiratory failure
- Chronic (esp poorly controlled asthma): airway remodelling → fixed/persistent airflow limitation that is NOT fully reversible (spontaneously or with bronchodilator therapy)
Prognosis
- Childhood-onset asthma (<18 yrs)
- Mild asthma (with infrequent wheezing) → often remits by adolescence
- Severe asthma (with frequent wheezing) → more likely to persist into adulthood
- Risk factors for persistence: atopy, parental asthma, later symptom onset, wheeze unrelated to viral infections, maternal/passive smoking
- Adult-onset asthma (≥18 yrs)
- Generally poorer prognosis than childhood-onset asthma [Ref]
Diagnosis
Clinical Features
Apart from a structured clinical history, specifically check for:
- Dry cough / breathlessness / chest tightness / reported wheeze / noisy breathing
- Any triggers that worsen symptoms
- Personal / family history of asthma or allergic rhinitis
Possible examination findings:
- Expiratory polyphonic wheeze
It is uncommon for a patient with stable asthma to present with a wheeze, which is more common when the patient is experiencing an exacerbation.
Even if the examination is normal, the person may still have asthma.
Diagnostic Tests (Objective Tests)
The choice of test and interpretation depends on the age group.
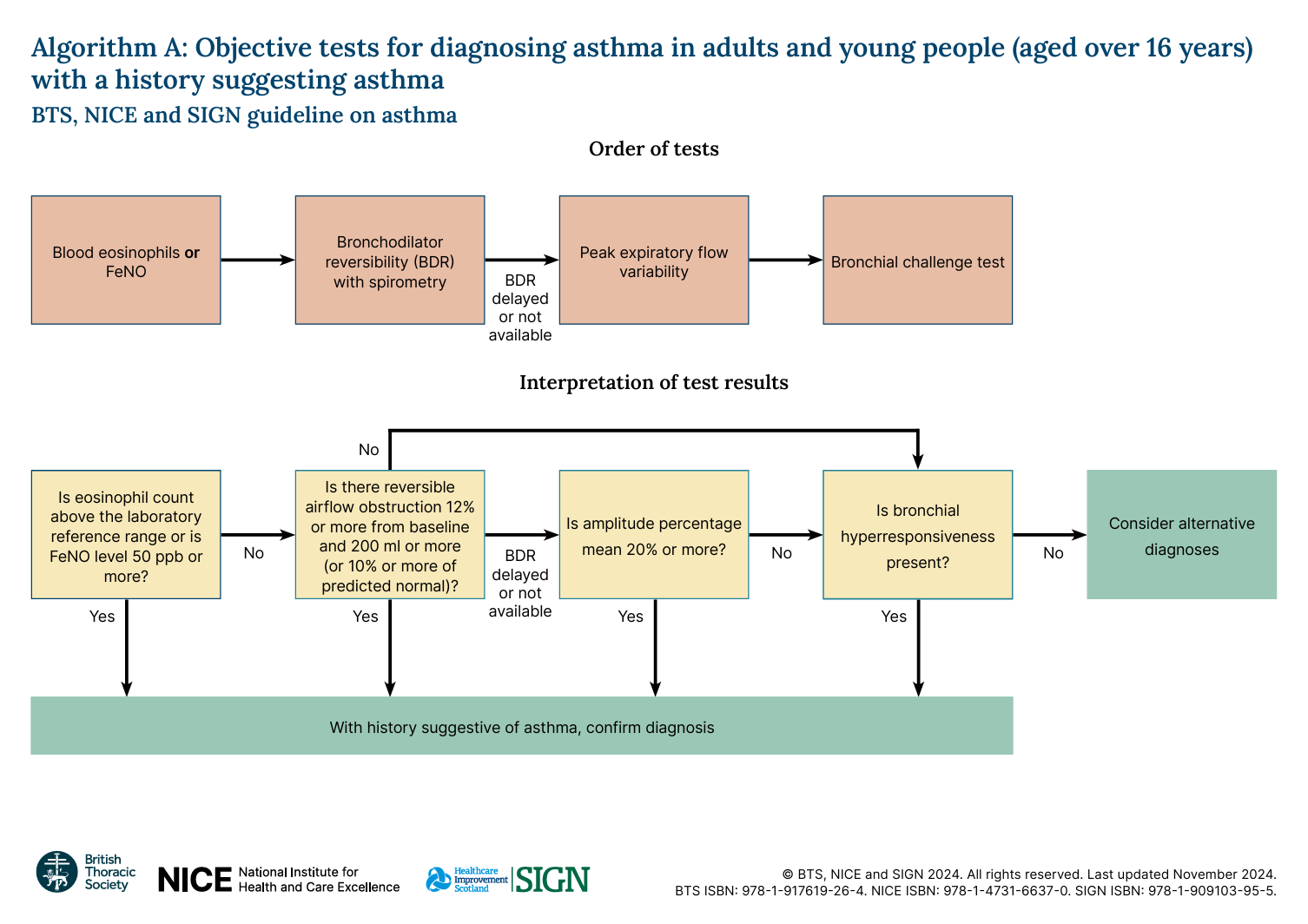
>16 y/o – Adults and Young People
1 positive test result from ANY of the following is sufficient to diagnose asthma (on top of clinical suspicion).
| Object tests | Positive test result | |
|---|---|---|
| 1st line | FeNO OR Blood eosinophil count |
FeNO ≥50 ppb OR ↑ Blood eosinophil count |
| 2nd line | Spirometry with BDR (preferred) | Post-bronchodilator FEV1 improvement by:
|
| Alternative:PEF for 2 weeks (twice daily) | PEF variability ≥20% | |
| 3rd line | Bronchial challenge test | Bronchial hyperresponsiveness |
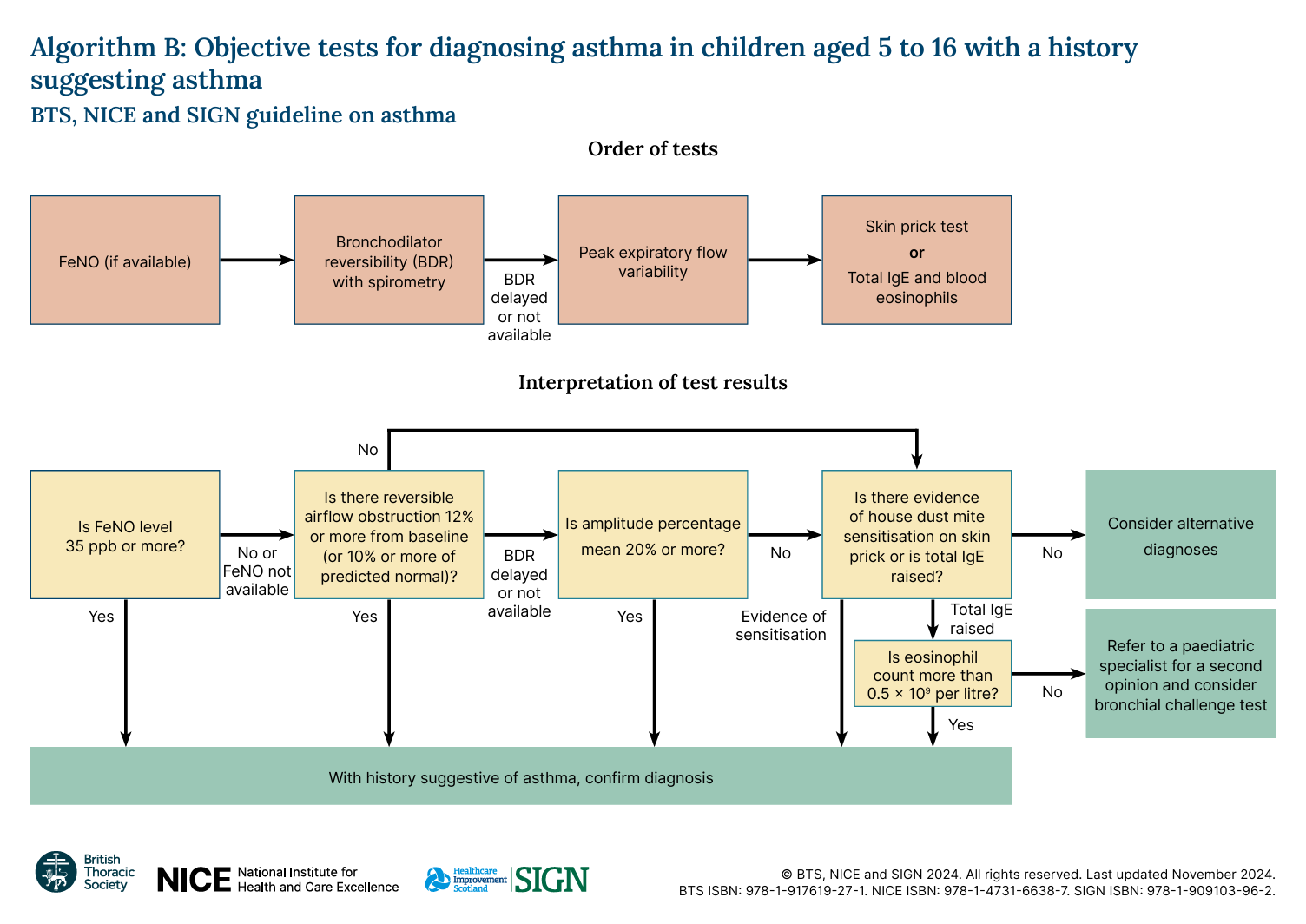
5 – 16 y/o – Children
1 positive test result from ANY of the following is sufficient to diagnose asthma (on top of clinical suspicion).
| Object tests | Positive test result | |
|---|---|---|
| 1st line | FeNO | FeNO ≥35 ppb |
| 2nd line | Spirometry with BDR (preferred)
|
Post-bronchodilator FEV1 improvement by:
|
| Alternative: PEF for 2 weeks (twice daily) | PEF variability ≥20% | |
| 3rd line | Skin prick test for house dust mite
OR Total IgE AND Blood eosinophil count |
Sensitive to house dust mite OR
↑ total IgE AND ↑ Blood eosinophil count (>0.5) **Exclude asthma if not sensitive to house dust mite OR total IgE not raised. |
<5 y/o
DO NOT perform object tests in <5 y/o, as it is difficult and there are no good reference standards.
If asthma is suspected clinically:
- Initiate treatment (see below)
- Review regularly
- If symptoms persist when they reach 5 y/o → attempt objective tests
If a child is unable to perform objective tests when they are aged 5:
- Re-attempt tests every 6 to 12 months
- Refer for specialist assessment if the child’s asthma is not responding to treatment
In children under 5 years old, it can be difficult to distinguish asthma from viral-induced wheeze, which many children outgrow. Definitive diagnosis is often deferred until the child is older and able to perform objective tests.
Asthma in young children may present less typically, with episodic cough and breathlessness, often triggered by viral infections and more noticeable at night.
Management
Pharmacological Management
It is important to recognise the definition of uncontrolled asthma, defined by ANY of the following:
- Any exacerbation requiring oral steroids
- Using reliever inhaler ≥3 days / week
- Night time waking ≥1 day / week
Features of uncontrolled asthma should always prompt assessment for poor adherence, incorrect inhaler technique, or inadequate treatment.
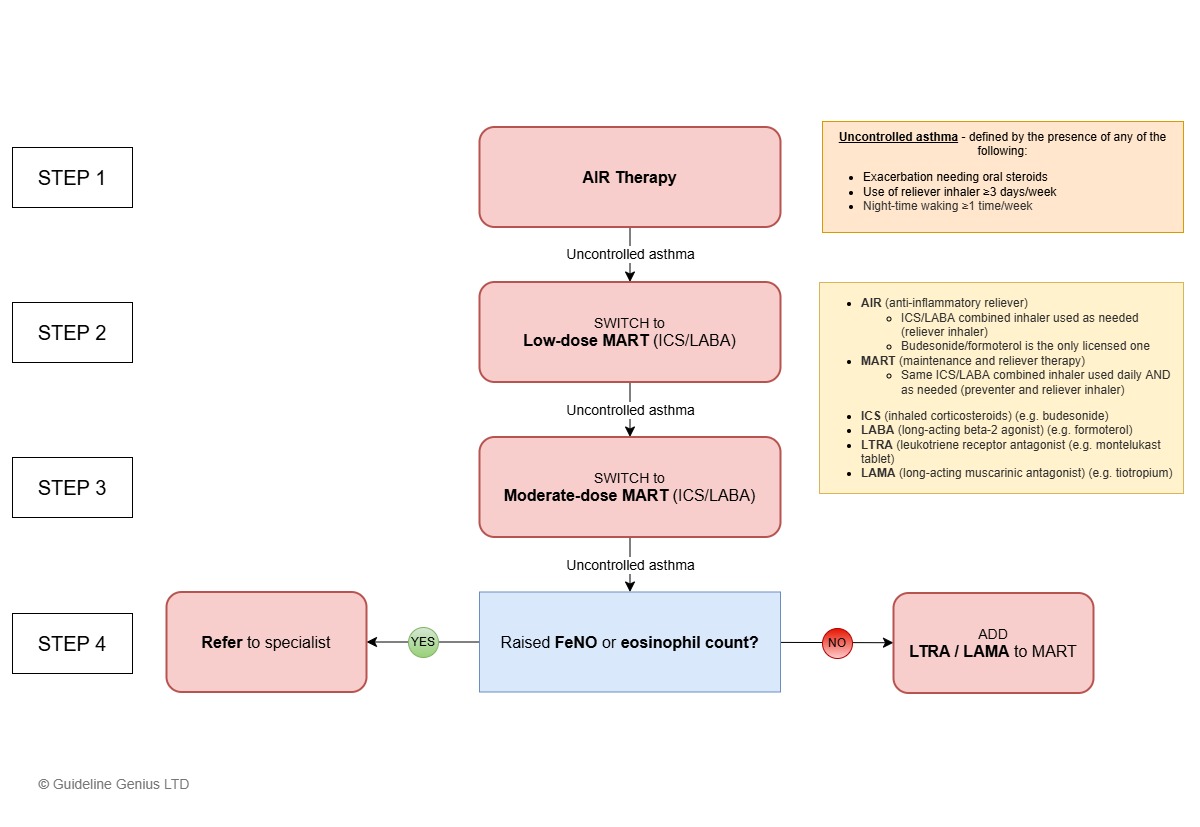
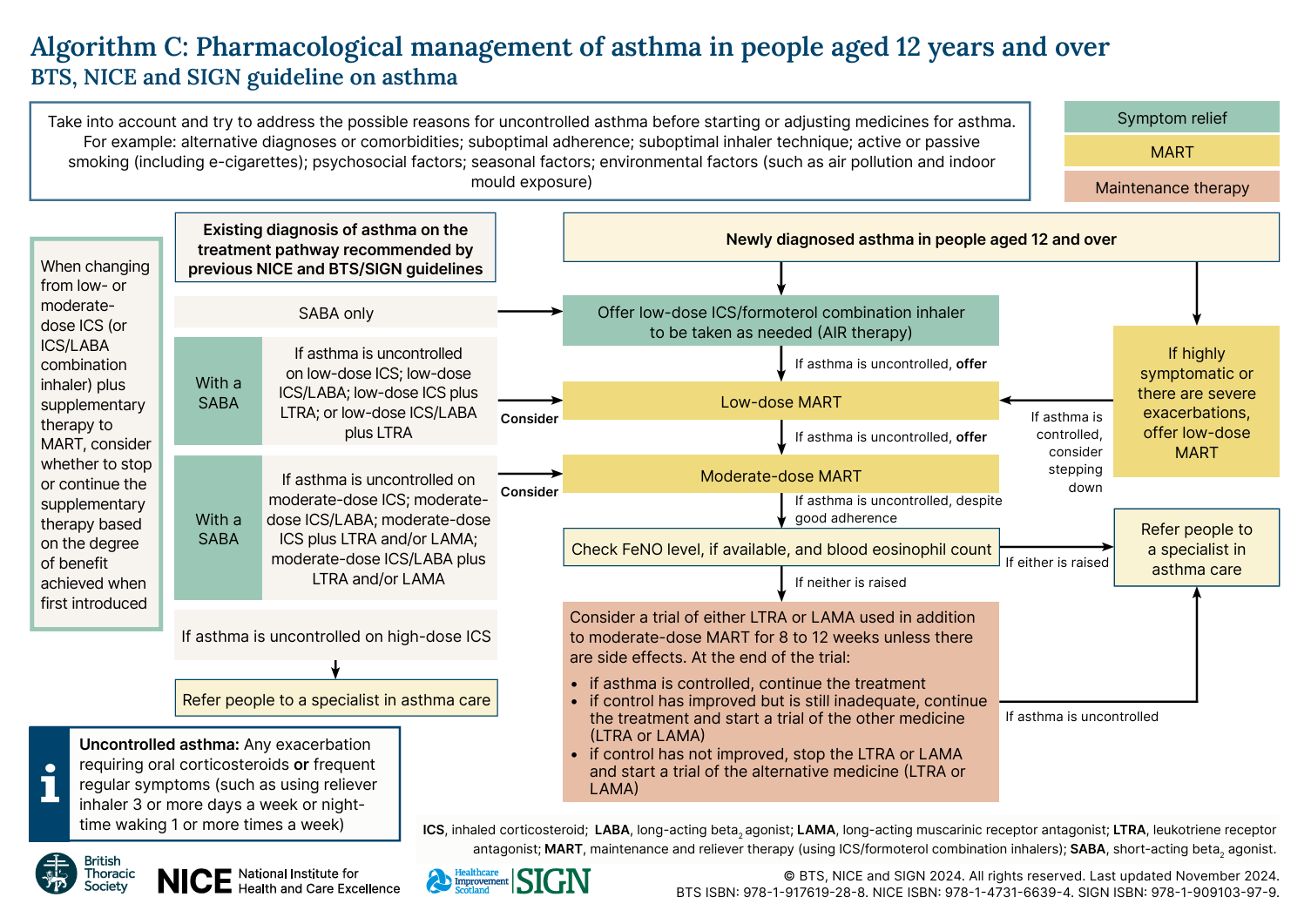
Management in ≥12 y/o – Flowchart
Rationale: At step 4 of the NICE asthma guidelines, FeNO and blood eosinophil count are used to identify persistent type 2 (eosinophilic) inflammation in resistant asthma.
Elevated FeNO or blood eosinophil count despite moderate-dose MART suggest severe asthma with type 2 inflammation. Although not explicitly mentioned in NICE guidelines, these patients are referred to specialist as the may benefit from biologics. UK-approved biologics for severe asthma with type 2 inflammation include:
- Anti-IgE (omalizumab) – for severe allergic IgE-mediated asthma
- Anti-IL-5 (mepolizumab, reslizumab, benralizumab) – for severe eosinophilic asthma
Management in ≥12 y/o
Step up the treatment when asthma is not controlled:
| Step 1 | Start AIR therapy with (budesonide/formoterol inhaler as needed) |
| Step 2 | Change to low-dose MART (low-dose ICS/formoterol inhaler) |
| Step 3 | Change to moderate-dose MART (moderate-dose ICS/formoterol inhaler) |
| Step 4 | Check FeNO and blood eosinophil count:
Subsequent steps
|
If a patient presents with highly symptomatic (e.g., regular nocturnal awakenings) asthma or a severe exacerbation upon first diagnosis → offer low-dose MART as step 1 (then consider stepping down afterwards).
Rationale: At step 4 of the NICE asthma guidelines, FeNO and blood eosinophil count are used to identify persistent type 2 (eosinophilic) inflammation in resistant asthma.
Elevated FeNO or blood eosinophil count despite moderate-dose MART suggest severe asthma with type 2 inflammation. Although not explicitly mentioned in NICE guidelines, these patients are referred to specialist as the may benefit from biologics. UK-approved biologics for severe asthma with type 2 inflammation include:
- Anti-IgE (omalizumab) – for severe allergic IgE-mediated asthma
- Anti-IL-5 (mepolizumab, reslizumab, benralizumab) – for severe eosinophilic asthma
AIR and MART Therapy
| Therapy | Description |
|---|---|
| AIR (anti-inflammatory reliever) therapy | To be used as a reliever / rescue therapy
|
| MART (maintenance and reliever therapy) | Involves a combined ICS/formoterol inhaler to be used:
|
AIR and MART essentially involve the same type of inhaler (ICS/formoterol) but are used differently:
- AIR to be used as needed (reliever inhaler)
- MART to be used as needed and daily (reliever and maintenance inhaler).
SABA monotherapy is no longer recommended
Transferring From Other Treatment Pathways
The table below gives summary guidance on how to transfer patients on other treatment pathways (including older guidance) to the current guidance.
| Existing Treatment | New Recommendations |
|---|---|
| SABA as needed | Switch to AIR as needed |
| Maintenance therapy including low-dose ICS | Switch to low-dose MART |
| Maintenance therapy including moderate-dose ICS | Switch to moderate-dose MART |
| Maintenance therapy including high-dose ICS | Refer to respiratory specialist |
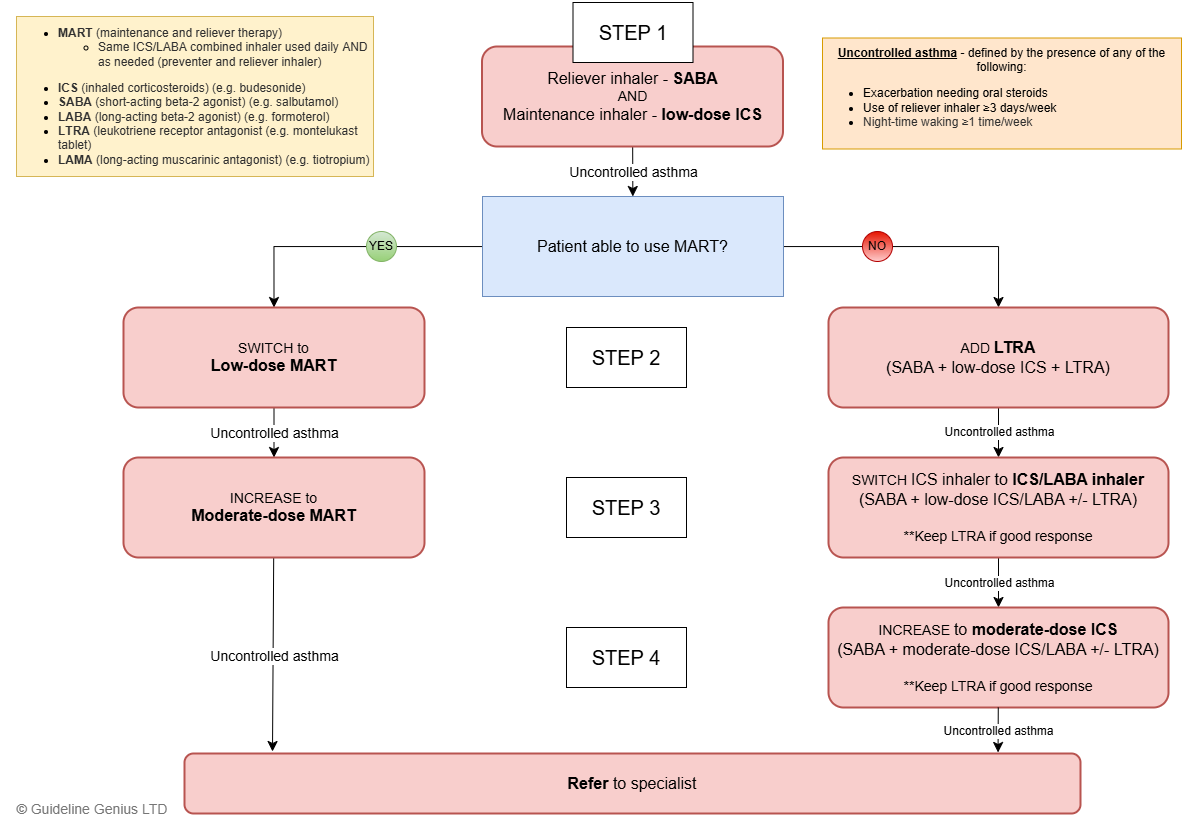
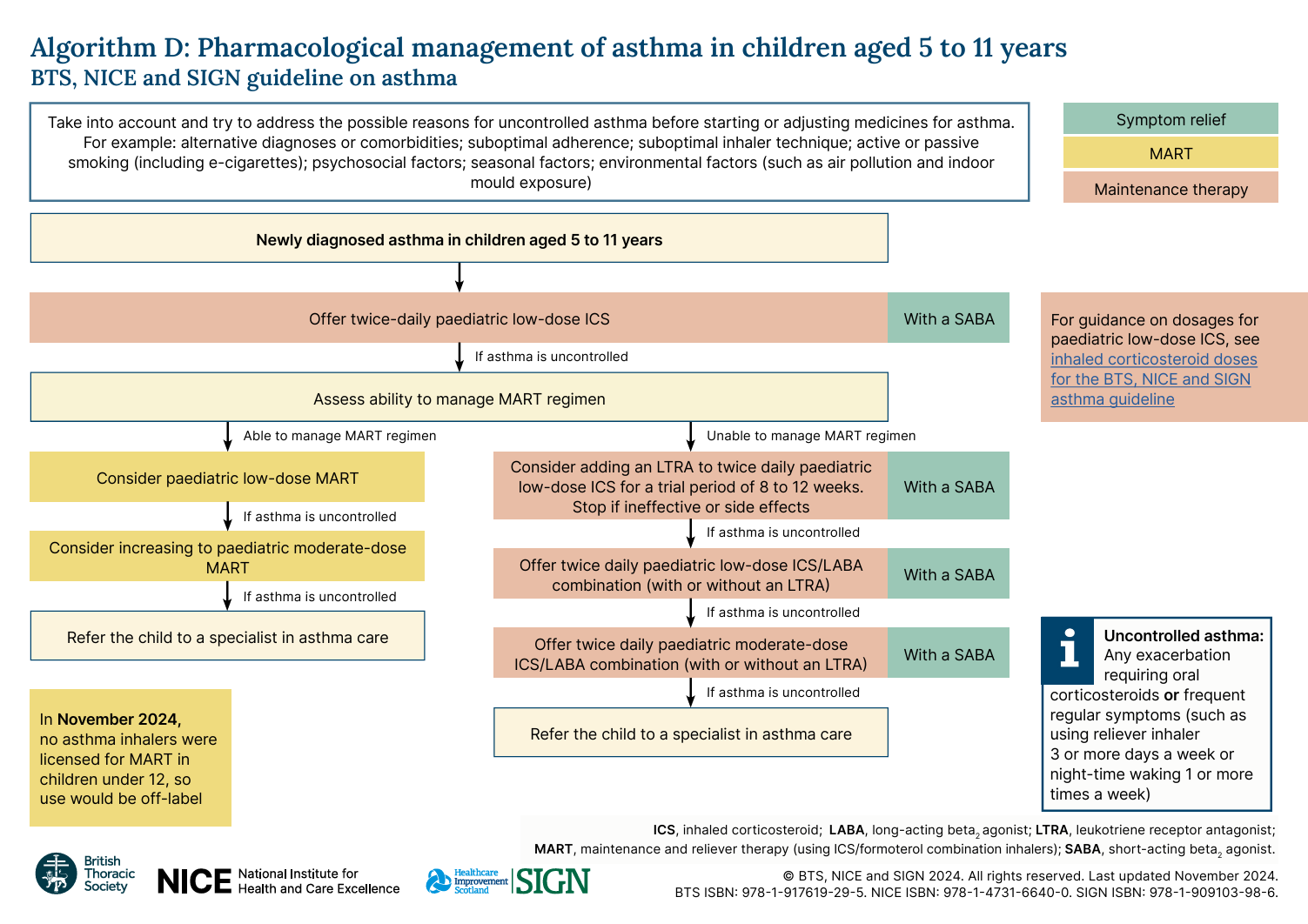
Management in 5-11 y/o
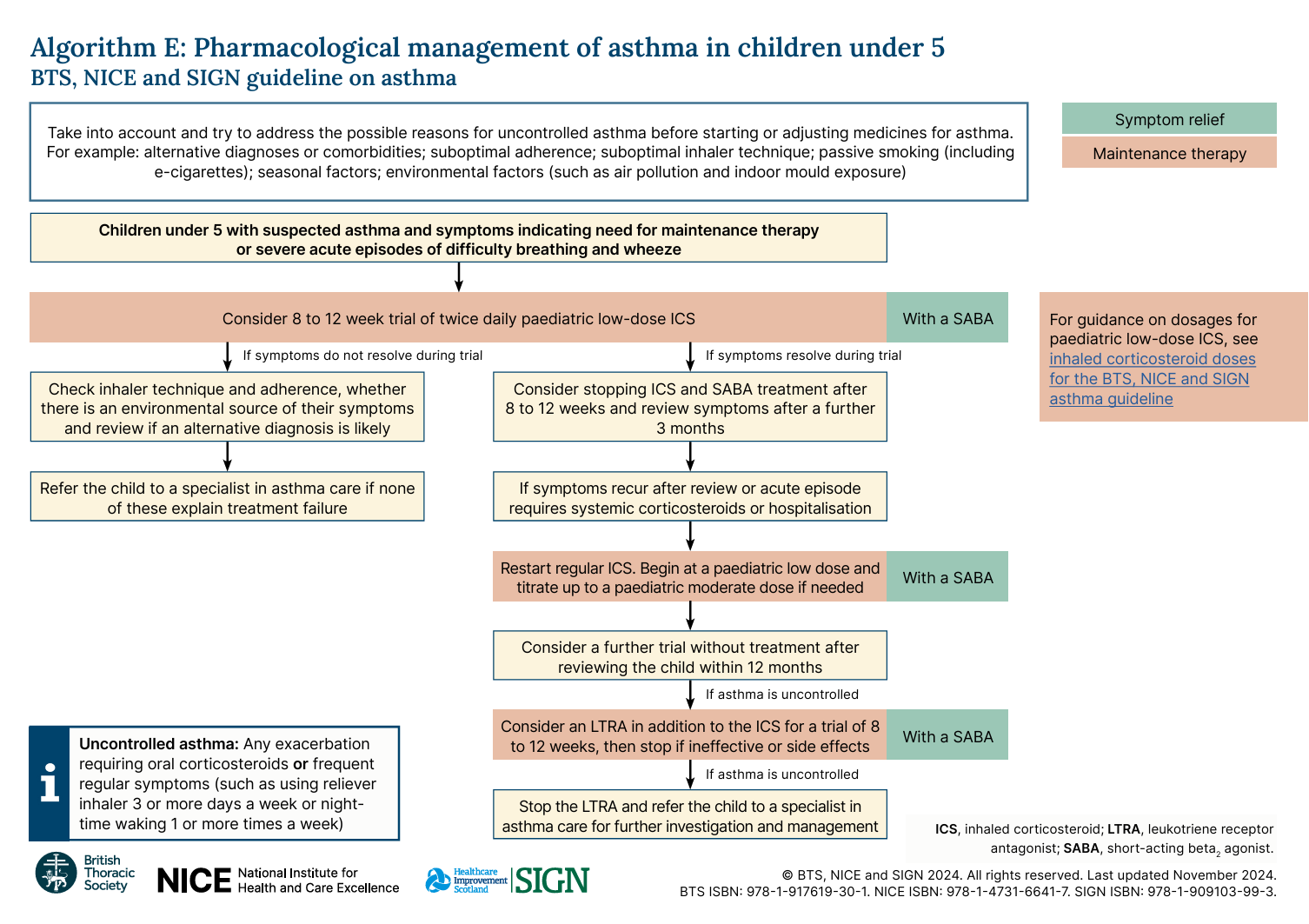
Management in <5 y/o
Consider the following for an 8-12 week trial:
- Maintenance therapy: paediatric low-dose ICS twice daily AND
- Reliever therapy: SABA as needed
If symptoms resolve during the trial → consider stopping the treatment after 8-12 weeks
For more details, see below for NICE’s algorithm.
Management in Pregnancy
Pregnancy
- Adequate asthma control is vital in pregnancy; asthma review is recommended during early pregnancy and postpartum
- The following can be safely taken during pregnancy:
- SABA and LABA
- ICS
- Oral theophyllines
- Oral corticosteroids (to treat exacerbations)
- NICE recommends that LTRA and LAMA should not be stopped if required to maintain adequate control
Breastfeeding
- Medications can be used as normal, in line with recommendations in the BNF
Reviewing Treatment
After starting or adjusting medicines for asthma, review the response to treatment in 8 to 12 weeks
Check FeNO level when asthma is uncontrolled, ↑ FeNO may indicate:
- Poor adherence to treatment, or
- Need to increase the dose of ICS
Follow Up and Monitor Asthma Control
Definition of complete control of asthma: (all must be present)
- No daytime symptoms
- No nighttime waking due to asthma
- No reliever inhaler use
- No asthma attacks
- No limitations on activity
- Normal lung function – FEV1 and/or PEF >80% predicted or best
- Minimal side effects from treatment
Follow-Up
At each appointment, check:
- Time off work / asthma due to asthma
- Usage of reliever inhaler (including adherence and inhaler technique)
- Number of oral corticosteroid courses
- Any presentation to emergency department / hospital admission due to asthma
Consider the following:
- Asthma Control Questionnaire / Asthma Control Test / Childhood Asthma Control Test
- FeNO – at review + before and after changing asthma therapy
DO NOT use regular PEF monitoring
Stepping Down Maintenance Therapy
Asthma should be well controlled on current therapy for a sustained period (typically ≥8–12 weeks) before reducing treatment.
In >12 y/o who are using low-dose MART or low-dose maintenance ICS + SABA as needed, step down to:
- As-needed AIR therapy – low-dose ICS/formoterol combination inhaler as needed
Occupational Asthma
Suspect occupational asthma in:
- Adult-onset asthma
- Poorly controlled established asthma
- Reappearance of childhood asthma
Screen occupational asthma with:
- Are symptoms the same / better / worse on days away from work
- Are symptoms the same / better / worse on time away from work, longer than usual breaks, at weekends, or between shifts
If occupational asthma is suspected → refer to occupational asthma specialist for serial PEF
Asthma in Pregnancy
Asthma management in pregnancy generally remains unchanged (both acute and chronic asthma):
- Patients should continue to use their usual asthma medications
- Focus on maintaining good asthma control
The risks of uncontrolled asthma outweigh the risks of treatment