Anaphylaxis
Resuscitation Council UK 2021 Emergency treatment of anaphylaxis: Guidelines for healthcare providers
Background Information
Definition
- Anaphylaxis: severe systemic type I hypersensitivity reaction (IgE-immune mediated) that is potentially life threatening
- Refractory anaphylaxis: persisting respiratory or cardiovascular symptoms despite 2 appropriate doses of IM adrenaline
- Biphasic anaphylaxis: recurrence of symptoms within 72 hours after complete recovery of anaphylaxis, in the absence of further exposure to the trigger.
Anaphylaxis should NOT be confused with anaphylactoid reactions (aka non-IgE mediated anaphylaxis, pseudoallergic reactions) [ref]
- Anaphylactoid reactions arise from non-immune (non-IgE) mediated activation of mast cells
- Examples
- Vancomycin infusion reaction (‘Red-man syndrome’)
- N-acetylcysteine infusion reaction
- Most contrast media reactions
- Still, anaphylactoid reactions are clinically indistinguishable from anaphylaxis, and are treated the same as anaphylaxis (with adrenaline)
Causes
Common triggers include:
- Food
- Most common trigger in children
- Nuts = leading cause
- Drugs
- Adults: most common trigger
- Most frequently
- Anaesthetics
- Antibiotics (esp. penicillin and cephalosporins)
- NSAIDs / aspirin
- Venoms (wasp & bee stings)
Other causes
- Idiopathic (significant portion of cases)
- Exercise induced → rare (~2%)
Risk factors for severe anaphylaxis
- Older age
- Concomitant mastocytosis
Complications and Prognosis
Complications
Airway & Respiratory
- Airway obstruction: due to angioedema of larynx/pharynx/tongue
- Bronchospasm & Respiratory failure
- Pulmonary oedema (non-cardiogenic)
Cardiovascular
- Distributive shock
- Cardiac arrest
Biphasic reaction
- Onset: within 1-24 hrs of initial reaction
Death
- Caused by
- Shock (~50%)
- Respiratory failure (remainder)
Prognosis
- Prognosis is generally good with prompt treatment; case fatality ratio <1%
- Higher mortality risk
- Pre-existing asthma (esp. poorly controlled)
- Delay or failure to use adrenaline
- Recurrence risk → previous reactions increase risk of recurrence
Clinical Features
The Resuscitation Council UK suggests that anaphylaxis is likely when ALL of the following are present:
- Sudden onset and rapid progression of symptoms
- Either one of the ABC problems – airway and/or breathing and/or circulation
- Skin and/or mucosal changes (e.g. urticarial rash)
In the absence of A/B/C problems, anaphylaxis is likely. In the presence of just urticaria, consider a simple allergic reaction.
Guidelines
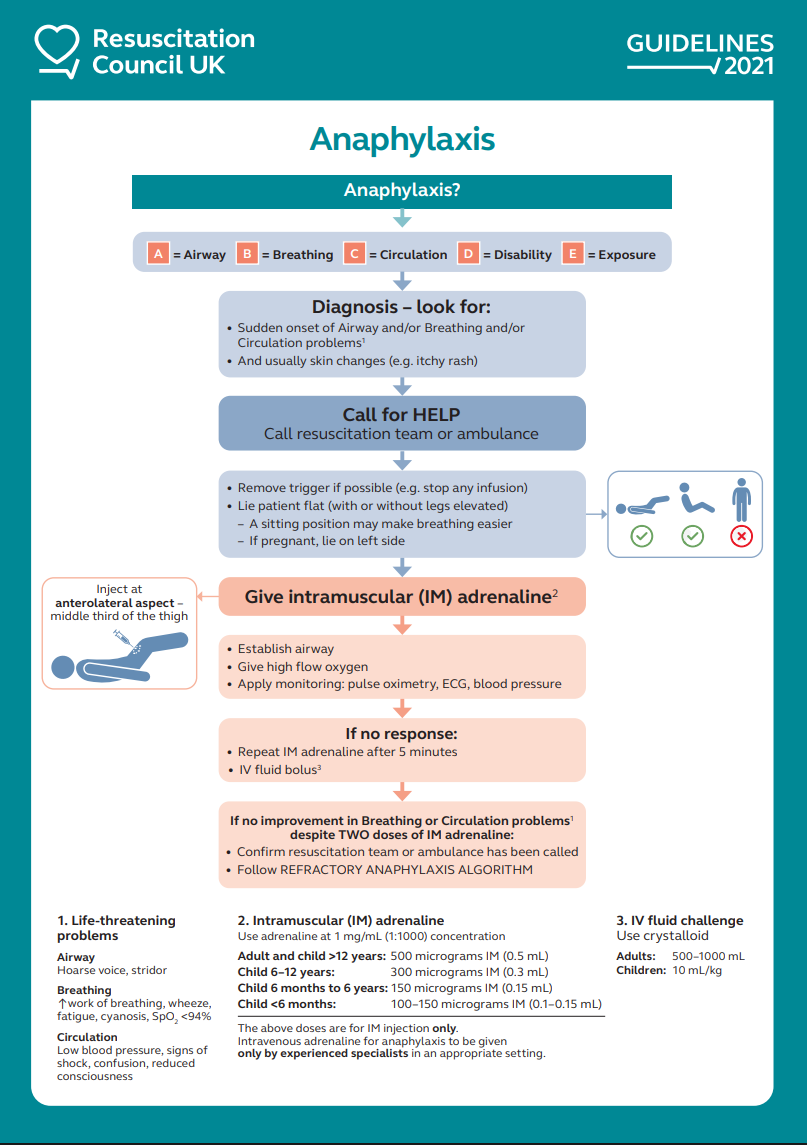
Management Algorithm
Apart from the ABCDE resuscitation measures, adrenaline is the single most important and high-priority management of anaphylaxis.
Initial Management
- Call for help
- Remove trigger if possible (e.g. stop any infusions)
- Reposition the patient
- Upright sitting position for patients with predominately breathing symptoms
- Supine position +/- leg elevation for patients with predominantly circulatory symptoms
Adrenaline Therapy
Give 1 dose of IM adrenaline in the anterolateral aspect of the middle-third thigh.
If no response after 5 minutes after 1st dose →
- Repeat IM adrenaline (2nd dose)
- Give IV fluid challenge with crystalloid
The Resuscitation Council UK guidelines recommend adrenaline to be always given via the IM route as the 1st line treatment for anaphylaxis, even if IV access is readily available. This is due to the greater risk of potentially life-threatening adverse effects from dilution error or incorrect dosing. IV adrenaline should only be administered by trained and experienced physicians like anaesthetists and intensive care physicians.
Adrenaline doses
Adrenaline dilution: 1 in 1,000 or 1 mg/mL
| Age | Dose | Volume |
|---|---|---|
| >12 y/o | 500 micrograms (0.5 mg) | 0.5 mL |
| 6 y/o – 12 y/o | 300 micrograms (0.3 mg) | 0.3 mL |
| 6 months – 6 y/o | 150 micrograms (0.15 mg) | 0.15 mL |
| <6 months | 100-150 micrograms (0.10-0.15 mg) | 0.10 – 0.15 mL |
Refractory Anaphylaxis Management
Seek specialist input to start low-dose IV adrenaline infusion
Before IV adrenaline infusion can be initiated, or if not appropriate:
- IM adrenaline to be given every 5 min
- Rapid IV fluid boluses
IV adrenaline infusion should only be given by an experienced specialist (e.g. intensive care physician, anaesthetist) in an appropriate setting.
Post-Emergency Treatment
Adjunct Therapy
The following medications do NOT form part of the initial emergency management of anaphylaxis. They have no role in treating the life-threatening complications of anaphylaxis, they should only be considered once the patient has been stabilised:
- Oral antihistamines (2nd generation, non-sedating) can be used to treat cutaneous symptoms from allergic reactions.
- Corticosteroids should only be considered for refractory reactions or ongoing asthma / shock.
Discharge and Follow-Up
Prior being considered for discharge, all patients should be kept for in-hospital observation for a minimum of 2-12 hours following resolution of symptoms.
A risk-stratified approach is recommended to decide the length of in-hospital observation that is warranted.
Prior discharge, all patients should be offered the following:
- Referral to a specialist allergy service
- Information about anaphylaxis, including how to recognise anaphylaxis and how to avoid the suspected trigger (if known)
- Educate on the self-management of anaphylaxis, including a prescription of 2 adrenaline auto-injectors, with appropriate training
- Information on the risk of biphasic anaphylaxis
- Information about patient support groups