Pneumothorax
NICE Guideline [NG39] Major trauma: assessment and initial management.
British Thoracic Society (BTS) Guideline for Pleural Disease 2023
Background Information
Definitions
Spontaneous pneumothorax: presence of air in the pleural space, between the visceral and parietal pleura, that occurs in the absence of trauma or medical intervention.
Tension pneumothorax is a life-threatening condition characterised by intrapleural pressure rises sufficiently to cause significant hemodynamic compromise, typically due to a one-way valve effect that traps air in the pleural space.
Aetiology
Causes of pneumothorax are classically divided into the following: [Ref1][Ref2]
| Category | Causes |
|---|---|
| Spontaneous pneumothorax | Spontaneous pneumothorax occurs spontaneously, without any preceding trauma / medical intervention.
Spontaneous pneumothorax can be sub-classified into:
|
| Traumatic pneumothorax |
|
| Iatrogenic pneumothorax |
|
Any type of pneumothorax can evolve into tension pneumothorax, however the risk is greater in traumatic and iatrogenic pneumothorax. [Ref]
Risk is highest in mechanically ventilated patients. [Ref]
Complication
Acute Complications
- Progression into tension pneumothorax
- Persistent air leak / failure of lung re-expansion
- Respiratory failure
- Obstructive shock (mostly seen in tension pneumothorax, where the mediastinal shift compresses the great veins and reduces preload)
Chronic Complications
- Recurrence is common (>50% recurrence risk after 1st episode, higher in the presence of underlying lung disease)
- Persistent air leak and failure of lung re-expansion
Diagnosis
Clinical Features
Symptoms
Sudden onset of:
- Pleuritic chest pain
- Dyspnoea
Signs
Typical respiratory examination findings:
| Examination aspect | Typical findings |
|---|---|
| Chest expansion | ↓ on the affected side (due to pain) |
| Percussion | Hyper-resonant over the affected area |
| Tactile fremitus | ↓ on the affected side |
| Auscultation | Reduced / absent breath sound over the affected area |
Additional findings that suggest tension pneumothorax:
- Haemodynamic instability
- Trachea deviation (away from the affected side) & Distended neck veins
- Typical signs but have low sensitivity
- Absence does NOT exclude diagnosis
Investigation and Diagnosis
1st line: chest X-ray
- Typical finding is a visible pleural line with lung markers only visible up to this line, no longer visible beyond the pleural line
- Ultrasound is increasingly used to identify pneumothorax (e.g. in eFAST)
2nd line (if chest X-ray is equivocal): CT chest
Tension pneumothorax should be a clinical diagnosis. Do not delay interventions to obtain imaging if tension pneumothorax is suspected.
Management
Tension Pneumothorax Management
Immediate management: chest decompression with needle decompression or finger thoracostomy
- Latest recommended site: 4th/5th intercostal space, mid-axillary line
- Traditional site: 2nd intercostal space, mid-clavicular line
Definitive management: chest drain insertion (insert a chest drain AFTER initial chest decompression)
Tension pneumothorax should be a clinical diagnosis. Do not delay interventions to obtain imaging if tension pneumothorax is suspected.
Spontaneous Pneumothorax Management
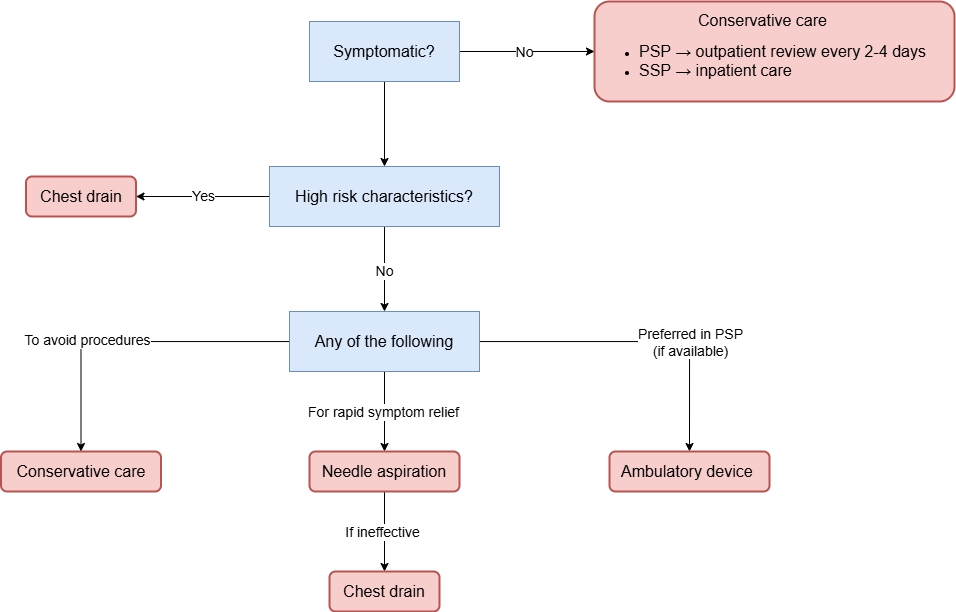
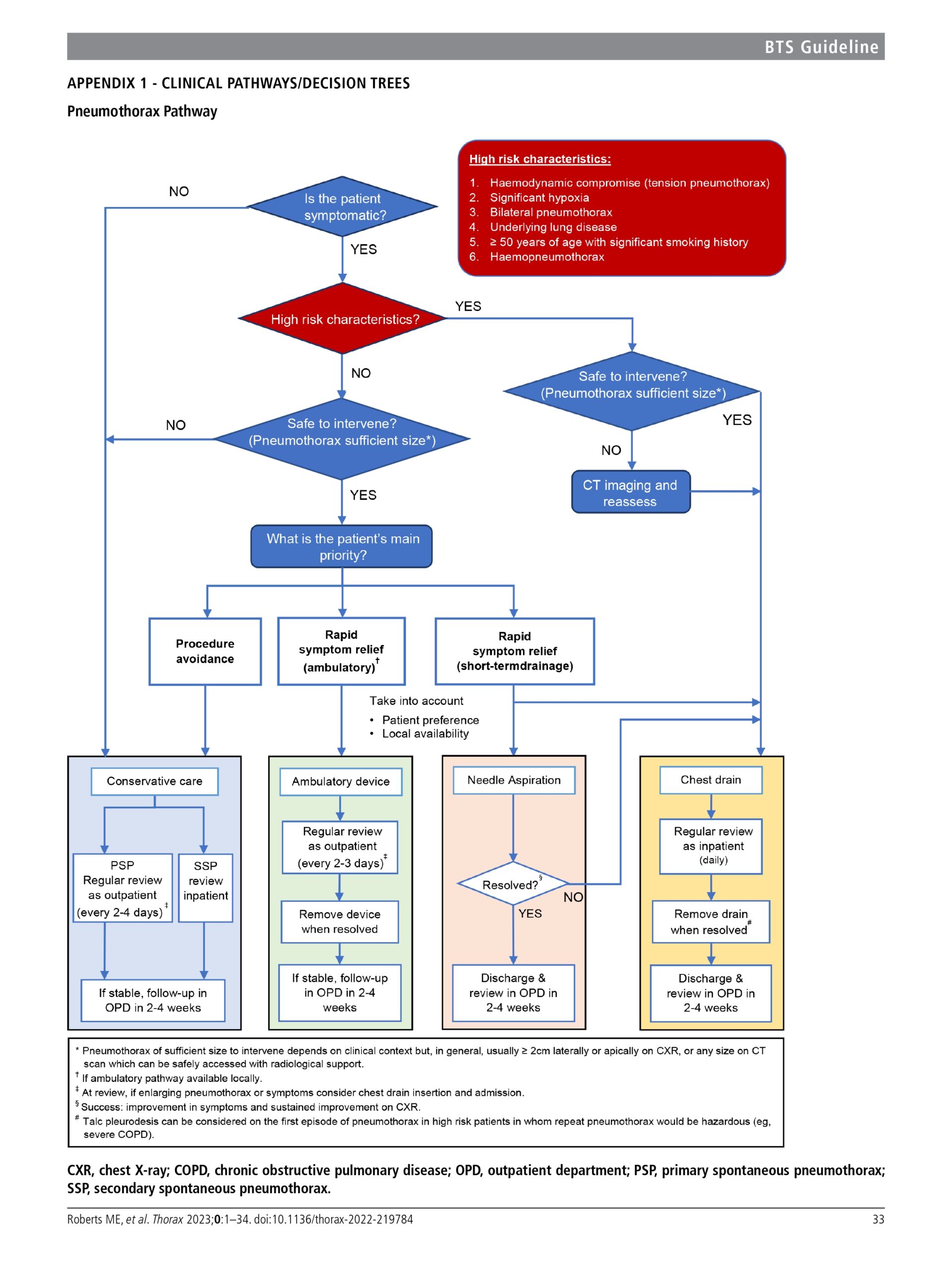
Full decision algorithm:
Symptomatic Pneumothorax
Assess for high-risk characteristics:
- Patient factors:
- ≥ 50 y/o with significant smoking history
- Presence of underlying lung disease (i.e. secondary pneumothorax)
- Significant hypoxia
- Pneumothorax factors:
- Haemodynamic compromise
- Bilateral pneumothorax
- Haemopneumothorax
Subsequent action, depends on whether high-risk characteristics are present or not.
High-Risk Characteristics Present
If safe to intervene → chest drain insertion
Subsequent care following chest drain insertion
- Admit as inpatient with daily review
- Remove chest drain when resolved
- Discharge and review as outpatient in 2-4 weeks
No High-Risk Characteristics
If safe to intervene → offer ANY of the following depending on the patient’s main priority
- If it is ‘safe to intervene’ → interventional options (i.e. needle aspiration / ambulatory device / chest drain) are allowed, but not mandatory
- However, if it is NOT ‘safe to intervene’ → interventional options should NOT be carried out
| Goal | Management pathway | Description |
|---|---|---|
| Patient wishes to avoid procedures | Conservative management |
|
| Rapid symptomatic relief | Needle aspiration |
|
| If locally available (preferred in PSP | Ambulatory device |
|
Asymptomatic Or Minimal Symptoms
Always offer conservative care regardless of pneumothorax size
- If PSP → discharge and review as outpatient every 2-4 days
- If SSP → admit as inpatient for a minimum of 24 hours with supplemental oxygen
Expected pneumothorax resolution time:
- 1cm pneumothorax → ~10 days
- 2cm pneumothorax → after 2-3 weeks
Post-discharge Advice
- Return to emergency department immediately if further breathlessness develops
- Advise smoking cessation to reduce risk of recurrence
- Patients can only fly 7 days after full resolution confirmed on CXR
- Patients should be advised to permanently avoid diving, unless a definitive preventive strategy has been performed (e.g., surgical pleurectomy)
References
ATLS® Advanced Trauma Life Support® Student Course Manual 10th Edition. 2018 American College of Surgeons.