Angle Closure Glaucoma
The Royal College of Ophthalmologists (RCO) Management of Angle Closure Glaucoma Guideline Jun 2022
NICE CKS Glaucoma Last Revised Fed 2023
Background Information
Definitions
- Glaucoma: visual field loss from optic neuropathy, commonly associated with raised IOP
- Angle-closure: narrowing/closure of the iridocorneal angle; most commonly due to contact/apposition of the peripheral iris and trabecular meshwork (irido-trabecular contact)
- The iridocorneal angle contains the trabecular meshwork, which is the primary pathway for aqueous humor drainage from the anterior chamber into Schlemm’s canal and subsequently out of the eye
- Angle-closure glaucoma (aka narrow-angle glaucoma): irido-trabecular contact with narrowing of the iridocorneal angle → rapid rise of IOP → optic neuropathy
Acute presentation of angle closure glaucoma is an ophthalmic emergency.
Guidelines
When to Suspect in Primary Care
This section is based on NICE CKS. RCO Guidelines only apply to secondary and tertiary care.
Suspect acute angle closure glaucoma in:
- Sudden onset red painful eye
- Previous episodes of eye pain, blurred vision, headaches, nausea and seeing halos around light (indicate intermittent angle closure episodes that self-resolved)
- Presence of a precipitating factor (any cause of mydriasis)[Ref]:
- dark room
- drugs (anticholinergic or adrenergic)
- stress or emotional arousal
O/E:
- Red painful eye associated with headache, N&V
- Hazy oedematous cornea
- Semi/mid-dilated, poorly reactive pupil (vertically oval shape)
- Tender hard eye
- ↑ IOP
If acute angle closure glaucoma is suspected → admit to ophthalmology immediately
Investigation and Diagnosis – Secondary and Tertiary Care
This section is based on RCO Guidelines.
Definitive investigation: gonioscopy (uses a slit lamp and lens to visualise the iridocorneal angle)
Other supplementary investigations:
- Tonometry – ↑ IOP
- Van Herick test – assessment of limbal anterior chamber depth (LAD)
- Anterior segment OCT
Management – Primary Care
This section is based on NICE CKS. RCO Guidelines only apply to secondary and tertiary care.
Refer immediately to be admitted under ophthalmology.
If immediate admission is not possible → start emergency treatment in primary care:
- Lie patient flat with face up, head NOT supported by a pillow
- Medications
- Antiemetic and analgesia if needed
- IOP lowering:
- Pilocarpine eye drops 2% / 4%
- Acetazolamide 500mg PO
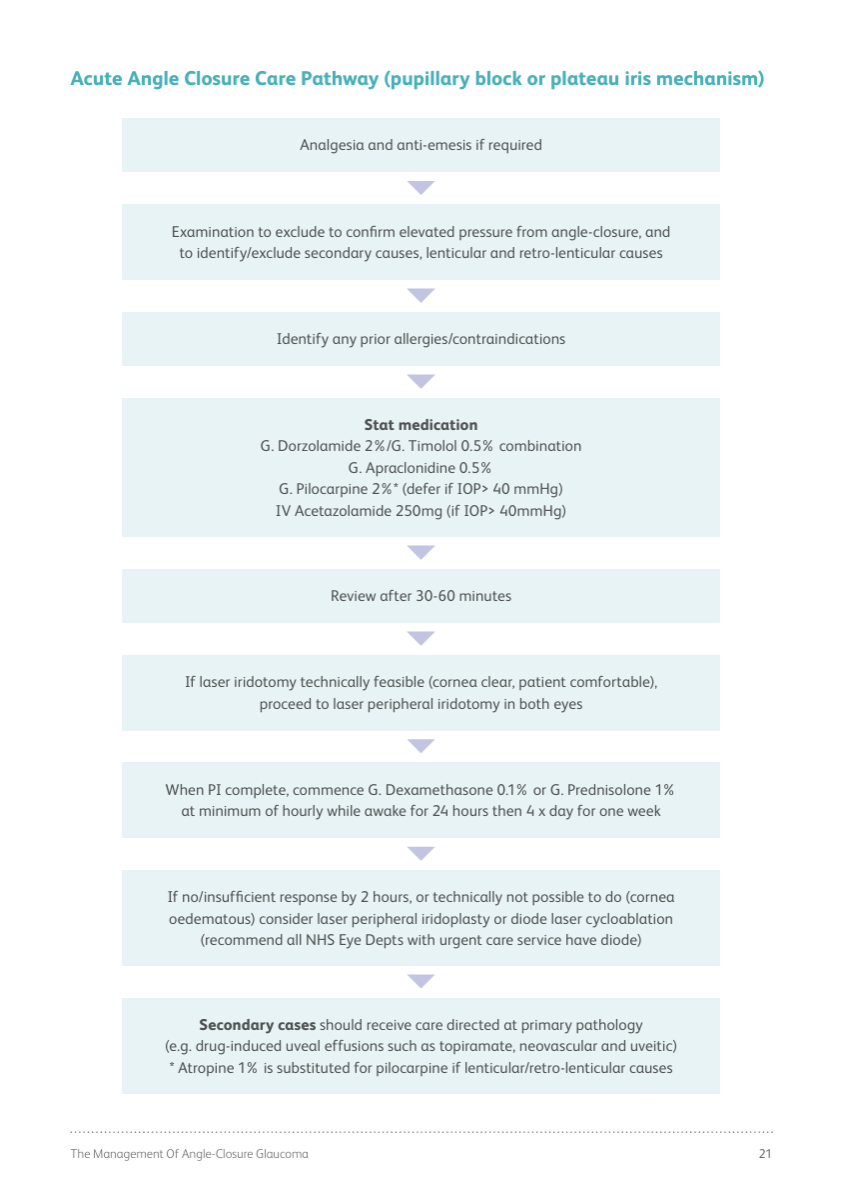
Management – Secondary and Tertiary Care
This section is based on RCO Guidelines.
- Analgesia and anti-emetics as needed
- Examination to confirm diagnosis + identify / exclude secondary causes
Stat medications (typically combination of eye drops PLUS systemic carbonic anhydrase inhibitor)
- Dorzolamide 2% + timolol 0.5% combined drops
- Apraclonidine 0.5% drops
- Pilocarpine 2% (if IOP >40 mmHg)
- IV acetazolamide 250mg (if IOP >40 mmHg)
Definitive management: laser peripheral iridotomy in both eyes
Management after peripheral iridotomy is completed:
- Steroid drops (dexamethasone 0.1% / prednisolone 1%)
- At least hourly for 24 hours, then QDS for 1 week
References
RCO – Acute Angle Closure Care Pathway
Original Guideline