Lyme Disease
NICE Guideline [NG95] Lyme disease. Last updated Oct 2018.
Background Information
Aetiology
Causative agent: Borrelia burgdorferi (spirochete)
Vector: various tick species
Risk factors (for tick exposure):
- Grassy and wooded areas
- South of England and Scottish Highlands
Clinical Features
Early localised Lyme disease – usually happens 7-14 days after tick bite:
- Flu-like symptoms (non-specific)
- Erythema migrans around tick bite
- Circular slowly expanding red ring with a central clearing
- Usually NOT itchy or painful or hot
Disseminated Lyme disease:
- Neuropathy (neuroborreliosis)
- Cranial nerve palsy (bilateral facial nerve palsy is common)
- Radiculopathy
- Peripheral neuropathy
- Arthritis
- Initial migratory arthralgia
- Late monoarthritis / asymmetric oligoarthritis
- Carditis
- AV block
- Myocarditis, pericarditis
Guidelines
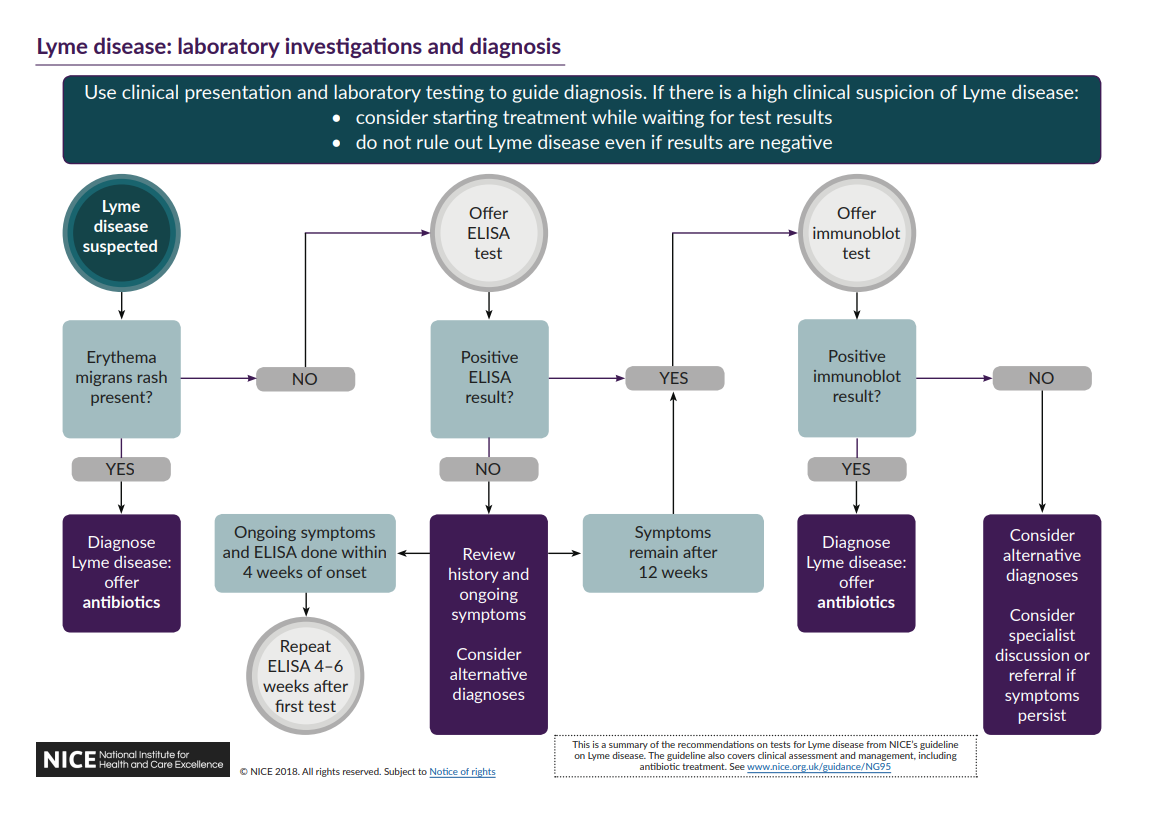
Investigation and Diagnosis
Diagnose and treat Lyme disease if:
- Erythema migrans present (no further testing needed), or
- Clinical suspicion + positive ELISA AND immunoblot test (see below for more details)
Erythema migrans is a circular, slowly-expanding red ring with central clearing that is usually NOT itchy, hot, or painful.
If the lesion is itchy / hot / painful, it is more likely to be a local reaction, instead of erythema migrans.
Diagnostic Approach
If erythema migrans is present → Lyme disease can be diagnosed without further testing.
If Lyme disease is suspected based on clinical features (without erythema migrans) → laboratory testing
- 1st line: ELISA (testing for antibodies against Borrelia burgdorferi)
- If +ve → immunoblot test
- If -ve → consider alternative Dx (if ongoing Sx and test done within 4 weeks of onset → repeat 4-6 weeks after)
- 2nd line: immunoblot test
- If+ve → diagnose Lyme disease
- If -ve → consider alternative Dx
Management
Approach
- Offer treatment if Lyme disease is diagnosed (i.e. erythema migrans / +ve laboratory testing)
- If <18 y/o → discuss with speicalist
Patients who are bitten by a tick and are asymptomatic (i.e. did not develop Lyme disease) do NOT require any treatment.
Choice of Treatment
Choice of antibiotics:
- 1st line: oral doxycycline for 21 days
- 2nd line: oral amoxicillin
Give IV ceftriaxone for 21 days if there is:
- CNS involvement, or
- Lyme carditis + haemodynamic instability
Be aware that doxycycline should NOT be used in children (BNF: only use in <12 y/o if there are no adequate alternatives); give amoxicillin instead as 1st line for Lyme disease.
Jarisch-Herxheimer Reaction
Jarisch-Herxheimer reaction is a treatment-related complication that can occur after treating Lyme disease (note it is most commonly associated with syphilis)
- Mechanism: systemic inflammatory reaction secondary to rapid destruction of spirochetes (Borrelia burgdorferi is a spirochete)
- Timing: between 1-12 hours after antibiotics are started
Clinical features:
- Fever
- Chills
- Muscle pain
- Headache
- Exacerbation of existing rash
Management:
- Self-limiting (usually resolves within 24-48 hours)
- Advise the patient to keep taking their antibiotics
- Supportive care
Jarisch-Herxheimer reaction is NOT an allergic reaction. However, it is important to be able to differentiate it from an allergic reaction (especially anaphylaxis).