Osteoarthritis (OA)
NICE guideline [NG226] Osteoarthritis in over 16s: diagnosis and management. Published Oct 2022.
NICE CKS Osteoarthritis. Last revised Dec 2023.
Background Information
Risk Factors
- Genetic contribution (independent of known environmental or demographic confounding factors)
- Biological factors
- Increasing age (typically >45 y/o)
- Women
- Overweight / obesity
- Low bone density
- Physical / biomechanical factors (causes of joint injury and damage)
- Joint laxity
- Reduced muscle strength
- Joint malalignment
- Exercise stresses
- Occupational stresses
Clinical Features
General Examination Findings
Possible findings include:
| Look |
|
| Feel |
|
| Move |
|
Findings in Knee OA
Typically bilateral and symmetrical.
Associated features:
- Giving way
- Locking
- Crepitus and tenderness along the joint line
- Restricted range of movement
Features seen in advanced disease:
- Bony swelling of the femoral condyles and lateral tibial plateau
- Varus deformity (more common than valgus)
- Antalgic gait
Medial tibiofemoral compartment knee OA is more common than lateral compartment OA.
Findings in Hip OA
- May present with deep pain in the anterior groin on walking or climbing stairs
- Painful restriction of internal rotation with the hip flexed
Features seen in advanced disease:
- Trendelenburg gait
- Fixed flexion external rotation deformity with compensatory lumbar lordosis and pelvic tilt
Findings in Hand OA
Typical joint involvement:
- 1st CMC joint
- PIP joint
- DIP joint
Other findings:
- Fixed flexion deformity of the CMC joint with hyperextension of the distal joints
- Squaring of the thumb
- Bouchard’s nodes (bony nodules next to the PIP joint)
- Heberden’s nodes (bony nodules next to the DIP joint)
In contrast to osteoarthritis, rheumatoid arthritis typically spares the DIP joints in the hands (+ feet).
X-ray in OA
Do NOT routinely use imaging to diagnose OA unless there are atypical features or features that suggest an alternative or additional diagnosis.
Typical radiological features of OA: (LOSS)
- Loss of joint space (or narrowing)
- Osteophyte formation
- Subchondral sclerosis
- Subchondral cysts
Note: structural changes on X-ray may not correlate with the presence or severity of symptoms or degree of functional impairment.
Complications
- Chronic pain
- Joint deformity
- Functional limitations
- Psychosocial impact
Guidelines
Investigation and Diagnosis
Clinical diagnosis of OA can be made if ALL of the following are present:
- ≥45 y/o
- Activity-related joint pain
- Morning joint stiffness lasting <30 min
Do not routinely use imaging to diagnose osteoarthritis unless there are atypical features or features that suggest an alternative or additional diagnosis.
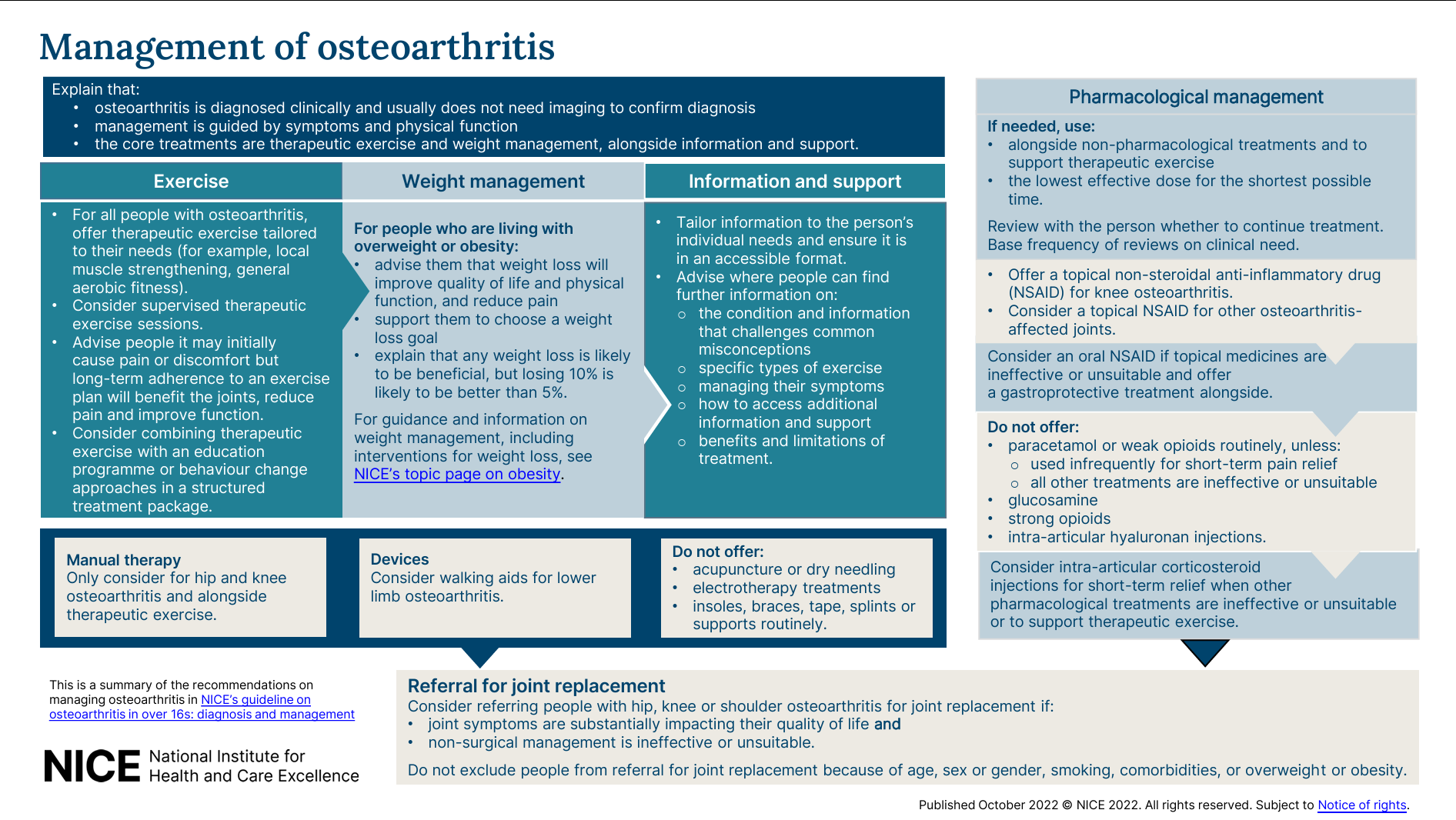
Management
General Advice / Conservative Management
Offer:
- Weight management – if the patient is overweight / obese
- Advise that any amount of weight loss is beneficial but losing 10% is likely better than 5%
- Therapeutic exercise tailored to patients (e.g. local muscle strengthening, general aerobic fitness)
Consider:
- Manual therapy in hip / knee OA alongside therapeutic exercise
- Walking aids if there is lower limb OA
Do not routinely offer an aid or device (insoles / braces / tape / splints / supports), unless there is joint instability or abnormal biomechanical loading AND therapeutic exercise is ineffective or unsuitable without it AND the addition of it is likely to improve movement and function.
NICE recommends NOT to offer:
- Acupuncture
- Dry needling
- Electrotherapy (including transcutaneous electrical nerve stimulation, ultrasound therapy, interferential therapy, laser therapy, pulsed short-wave therapy, neuromuscular electrical stimulation)
Pharmacological Management
Pharmacological management should always be used alongside non-pharmacological options and at the lowest effective dose for the shortest possible time:
- 1st line: topical NSAID (useful for knee OA, but maybe less effective for other OAs)
- 2nd line: oral NSAID with gastroprotection
- 3rd line: paracetamol or weak opioid for short-term pain relief and infrequent use only
- 4th line: intra-articular corticosteroid injections (explain that it only provides 2-10 weeks of pain relief)
NICE recommends NOT to offer:
- Glucosamine (explain there is no strong evidence of benefit)
- Strong opioids (explain that the risks outweigh the benefits)
- Intra-articular hyaluronan injections
Surgical Management – Joint Replacement
Consider referring patients with knee / hip / shoulder OA for shoulder replacement if:
- Symptoms are substantially impacting quality of life, AND
- Non-surgical management is ineffective / unsuitable
Do not exclude people with OA from referral for joint replacement because of:
- Age
- Sex or gender
- Smoking
- Comorbidities
- Overweight or obesity, based on measurements such as body mass index (BMI).
NICE recommends NOT to offer arthroscopic lavage or debridement for OA.
References
NICE Visual Summary – Management of Osteoarthritis
Original Guideline